Welcome To
Odisha Regional Study Point
We Allows the best competitive exam preparation for SSC,BANKING, RAILWAY &Other State Exam(CT, BE.d) DECE(IGNOU) In ଓଡ଼ିଆ Language…
Why opt ORSP?
✅Daily Free Live class
✅Daily Free practice Quiz
✅FREE Live Tests Quiz
✅Performance Analysis
✅All Govt Exams are Covered
Join With us As per Schedule
And
Happy Learning…
Thank You
ORSP
(9502052059)
DECE-2 (PREVIOUS YEAR QUESTION-IGNOU-ORSP)
DECE 2 (Important Questions)(ENG)-IGNOU-ORSP
DECE 2 (Important Questions)(HIN)-IGNOU-ORSP
Protins-
Protein is a macronutrient that is essential to building muscle mass. It is commonly found in animal products, though is also present in other sources, such as nuts and legumes.
There are three macronutrients: protein, fats and carbohydrates. Macronutrients provide calories, or energy. The body requires large amounts of macronutrients to sustain life, hence the term “macro,” according to the University of Illinois McKinley Health Center. Each gram of protein contains 4 calories. Protein makes up about 15 percent of a person’s body weight.
Chemically, protein is composed of amino acids, which are organic compounds made of carbon, hydrogen, nitrogen, oxygen or sulfur. Amino acids are the building blocks of proteins, and proteins are the building blocks of muscle mass, according to the National Institutes of Health (NIH).
“When protein is broken down in the body it helps to fuel muscle mass, which helps metabolism,
DECE 2 (Important Questions)-IGNOU-ORSP
(WHO) (1948) definition of health, which is as follows:
“Health is a state of complete physical, mental and social well-being and not merely
an absence of disease or infirmity.”
In recent years, this definition has been expanded to include the ability to lead a
“socially and economically productive life”.
some limitations. Can you identify them? Yes, one drawback is the absence of
measurable terms. For instance, can we measure the “mental well-being” or the
“social well-being” of a person and decide if it is complete? Well, not really!
Another criticism is that health cannot be defined as a “state”. Instead, it must be
seen as a process of continuous adjustment of people to the changing environment
and demands of life.
Further, many consider that health, as defined by WHO, is an idealistic goal rather
than a realistic one. There are times when we are suffering from an infection or
concentrating on our work, or worried about something. How often can we claim to
be in a state of complete physical, mental and social well-being? Some consider the
WHO definition irrelevant to everyday demands as nobody qualifies as healthy.
That is, if we follow this definition, most of us are sick!
However, in spite of the limitations mentioned above, the concept of health as
defined by WHO is broad and positive in its implications. It sets out the standard;
the standard of “positive health”, towards which all of us should strive.
Now what is positive health? You know that the WHO definition of health
envisages 3 dimensions of health-physical, mental and social. A person who enjoys
health at all these three levels is said to be in a state of positive health. The concept of
positive health implies the notion of “perfect functioning of the body and mind in the
social environment”. In such a state, biologically, every part and organ of the body is
functioning at optimum capacity and in perfect harmony; psychologically, the
individual feels a sense of well-being, and socially, her capacities for participation in
the social system are optimal.
Ans.
we shall take a look at some of the newer dimensions of health spiritual and
vocational. As we shall see, all these dimensions are closely related and interact
with, each other.
organ is functioning at optimum capacity and in harmony with the rest of the body.
It is a very important component of health. And in fact, in practical terms, generally
when we say that a person is healthy, we are referring to this dimension. Physical
health is comparatively easy to identify and describe.
Some of the signs of physical well-being of a person are:
Lustrous hair

Healthy scalp


Clean skin

Bright, clear eyes

No malformations of skeleton
Weight normal for height and age
Well developed and firm muscles
Smooth, easy, coordinated body movements
Regular activities of bowels and bladder
Good appetite

Sound sleep

all the senses (such as sight and hearing) are intact.
Physical health can be assessed by measures such as clinical examination, dietary
and nutritional assessment and laboratory investigations. You must be aware that it
is this dimension of health that has been receiving the most attention.
Mental Dimension: Mental health is a vital component of total health. It is basic for
dealing effectively with reality, with oneself and with others. Only a mentally
healthy person is able to meet her life problems in such a way as to provide her with
a feeling of personal satisfaction and to contribute satisfactorily to the welfare of the
society. A person who is mentally healthy is one who is free from unsolvable
internal conflicts and is able to arrive at decisions is confident about her own abilities
but recognizes her faults has high self-esteem assumes responsibilities according to
her capacity and finds satisfaction in their accomplishment is not in the habit of
condemning or pitying herself all the time is able to handle any situation without
getting too upset or tense has good control over her emotions and does not give in
frequently to strong feelings of fear, jealousy, anger or guilt adapts to situations and
people is sensitive to the emotional needs of others deals with others with
consideration is well adjusted and gets along well with others.
when she is the boundaries are not that clear. What would you say about somebody
who lacks self-esteem or is indecisive? The extent is obviously an important
criterion And as is true of health in general, mental health is not simply the absence of mental
illness. So what is important is not just the absence of negative attributes, but the
presence of positive ones. As things stand, our knowledge of mental health is still
incomplete and we do not have precise tools for measuring mental health.
body. Poor mental health affects physical health and vice-versa.
Psychological factors play a major role in physical disorders
bronchial asthma

from a chronic kidney problem or a congenital heart condition. Her health condition
is likely to influence her activity level, her schooling and her friendships.
A healthy person should be well adjusted in the community of which she is a part
and should be able to function for the betterment of her community.
The social dimension of health includes the person’s ability to see herself as a
member of a larger community, the quantity and quality of her interpersonal
relationships with others and the extent of her involvement with the community.
She should fulfill her social obligations. These include obligations to the family as
well as the community. In addition, she should be able to relate to others, that is,
help others and get along well with them.
As in the case of mental health, while extreme forms of social ill-health are easy to
identify, the same is not true of minor deviations. All of us would recognize
criminals as socially ill individuals, and acts like theft and murder as manifestations
of social ill-health, but when it comes to areas like fulfilling one’s responsibility and
ability to get along well with others, the line between normal and abnormal gets
nebulous.
need better yardsticks to measure this dimension of health. The three aspects of
health, that is, physical, mental and social well-being, mentioned in the WHO
definition, are closely interrelated. Change in any one of them is normally
accompanied by changes in the other aspects too. For example, recall how your
mental and social well-being had been affected when you had been ill! Similarly, if
you are very tense about something, you may lose your appetite and gradually, your
physical well-being may get influenced. The way you interact with others may also
get affected.
Let us now take a look at two more dimensions of health, which are not mentioned
in the WHO definition. These are the spiritual dimension and the vocational
dimension. Though still not precisely defined, these dimensions are fast gaining
recognition. A few other dimensions have also been suggested such as philosophical,
cultural, environmental and educational, but we shall not go into these.
health, it is being widely believed that time has come to give serious consideration to
the spiritual dimension and to the role it plays in health and disease. Spiritual health,
in this context, refers to the striving to understand the meaning and purpose of life.
It is that “something” which goes beyond physiology and psychology. As you can
observe, spiritual health does not really lend itself to a concrete definition. But it
does include integrity, principles and ethics, belief in concepts that may not have a
scientific explanation, commitment to some higher being and a feeling of being
linked to the whole universe to comprise, as mentioned earlier, a perception of the
meaning and purpose of life.
relatively new concept and because of its very nature, has yet to acquire a precise,
universally accepted definition. What is not in doubt however, is the need to pay
attention to this aspect, particularly in view of the stresses and strains of modern life.
A person has to be at peace with her-self before she can be at peace with the world!
life of the health of the individual is now being realized. To understand the
importance of this dimension, just think of the possible repercussions for the
individual when she suddenly loses her job.
When work that a person does for a living is adapted to the goals that she has set for
herself, her capabilities and her limitations, it often plays an important role in
promoting physical and mental health, and hence the other aspects as well. In other
words, it contributes to the total health of the individual. Doing the work well is a
source of satisfaction and self-esteem.
For many, the vocational dimension may only be a source of income. To others, it
may be the visible result of the efforts of the other dimensions and represent what
the person considers “success” in life. For most, both are relevant. At the same time,
it is not necessary that a person must earn money in order to achieve a sense of
fulfillment. Many may find satisfaction in doing things that do not bring financial
returns.
The vocational aspect influences and-is influenced by the other dimensions of health.
This, as you are well aware, is in fact true of each aspect of health.
better one. What effects is this likely to have as far as her overall health is concerned?
Well, she is likely to feel frustrated all the time, with accompanying feelings of
anxiety, anger and/or low self-esteem. Her constant state of tension may affect her
physical health. Her likely irritability may also affect her social health.
but these are strong possibilities. Don’t you agree?
Q4. Describe the processes of digestion, absorption and utilization of food.(10 MARK)
Ans. Digestion of Food: Let us now take a look at the overall process of how
digestion occurs. Digestion takes place step-by-step at various sites in the digestive
tract as you will learn from the following discussion,
Mouth: As you have already noticed, the process of digestion begins in the mouth
where food is chewed by the teeth and mixed with saliva. While the food is still in
the mouth, it is acted upon by an enzyme, which acts only on cooked carbohydrates
such as starch and partially digests them or breaks them up into smaller units.

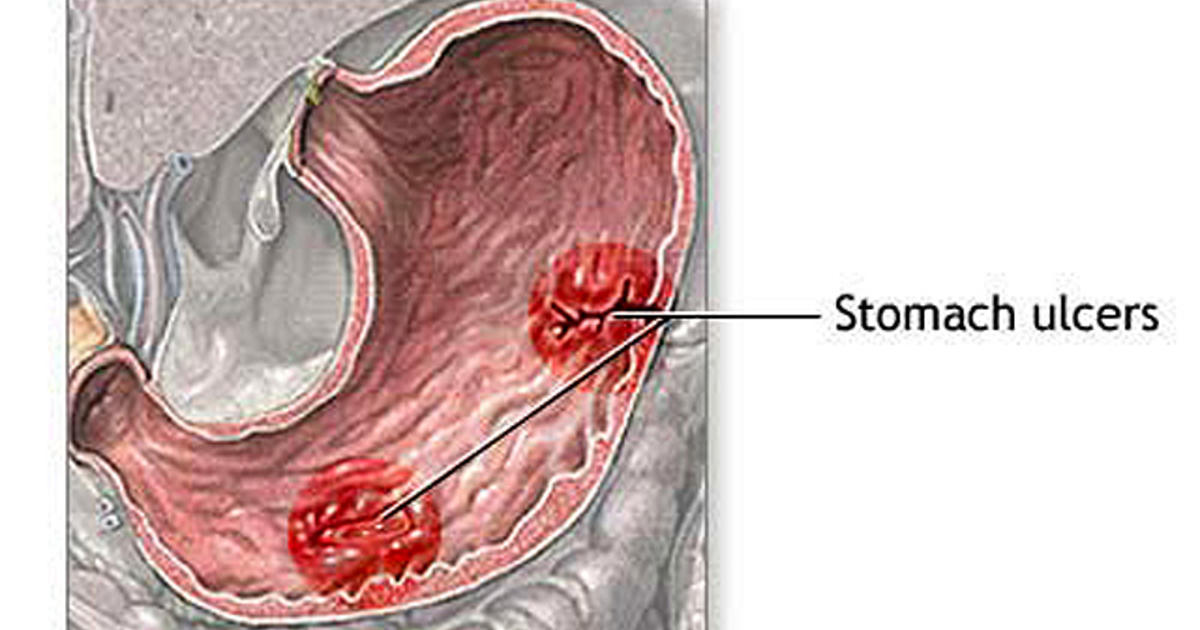
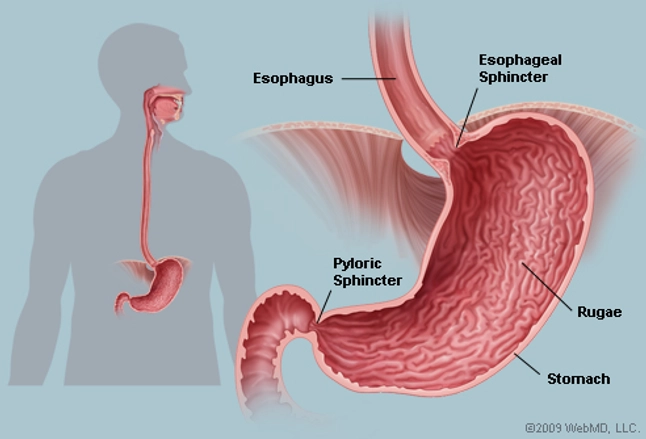
Stomach: The chewed food mixed with saliva then passes into the stomach through
the tube-like structure called the esophagus. Here it gets mixed with the digestive
juice present in the stomach called gastric juice which is acidic in nature. Mixing of
food with the gastric juice converts the food into a thin soup-like consistency. Gastric
juice contains an enzyme which acts on proteins and brings about their partial
digestion. Other nutrients in food remain chemically unchanged.
Small intestine: The next stop in the digestive tract is the small intestine. The
partially digested mass of food passes from the stomach into the small intestine. The
small intestine not only contains intestinal juice (which is secreted from the small
intestine itself) but also secretions from the liver and pancreas. The secretion from
the liver is called bile and from the pancreas is known as pancreatic juice. Bile aids in
the digestion and absorption of fats (you will learn about the role of bile in fat
digestion in the next Unit). Both pancreatic and intestinal juices contain enzymes
which break down fats, proteins and carbohydrates into simpler substances. These
simple substances ultimately reach the bloodstream.
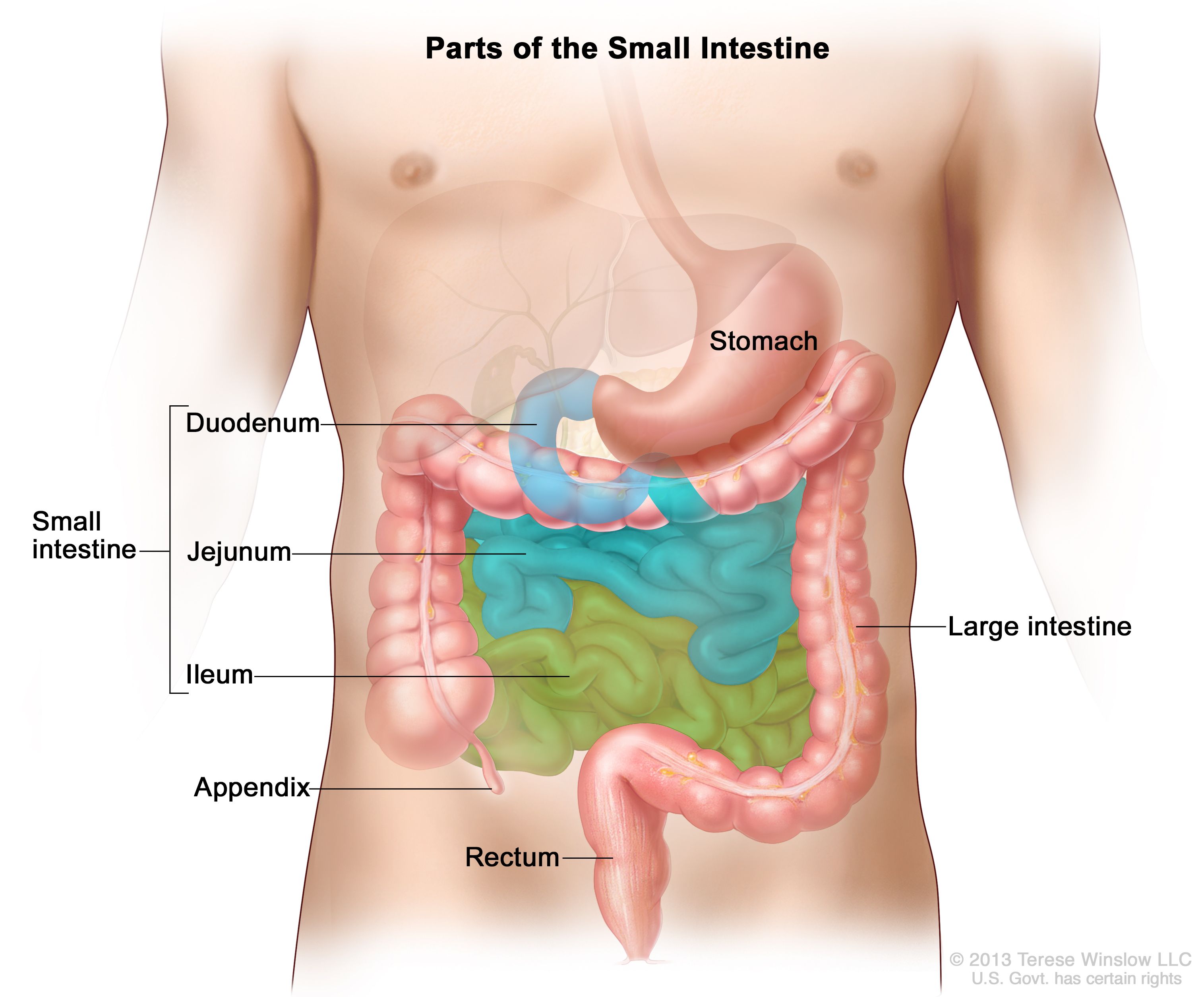
Large intestine: The components of food which are not absorbed in the small
intestine along with a large amount of water passes on to the large intestine. Here,
most of the excess water is reabsorbed and the remaining water and solid matter is
eliminated from the body as fasces,

Absorption of Food: Where is food absorbed? You would have realized by now that
absorption takes place in the small intestine. The end products of digestion or the
nutrients present in the small intestine can be used by the body only when they enter
the bloodstream. This process of movement of digested food or nutrients across the
intestinal wall to the bloodstream is termed absorption of food. The wall of the small
intestine is made up of numerous folds or finger-like projections known as villi. The
presence of these villi tremendously increase the total area from which absorption
can take place. Most of the nutrients are absorbed from the upper part of the small
intestine though some are absorbed from the lower portion

As you know, the end products of digestion move into the bloodstream. The blood
circulating in the body and therefore, the nutrients it carries reaches every cell of the
body. Once they reach the cell, the nutrients perform their specific functions.
Utilization of Food: How is food utilized? In order to be utilized for specific
functions the absorbed end products or the nutrients from the food we eat further
undergo chemical changes. They are either further broken down to release energy or
are used to -form more complex substances. We use a certain term to refer to these
processes. Let us learn this term.
Metabolism is a general term. It refers to all the chemical changes that take place in
the cells after the end products of digestion are absorbed. You know it is of two
types breakdown of complex substances into simpler ones and manufacture of
complex substances from simple ones.
Carbohydrates are a combination of oxygen, hydrogen, and carbon that are packed into starch, sugar or fibre. Carbohydrates are of two types, available and non-available.
Explanation:
Available carbohydrates are starch and sugar that are energy sources for the body. They are broken down into glucose and utilized by the body in different bio-chemical reactions.
Non-available ‘carbohydrates are not digested’ and absorbed by the body. They are fibres that are helpful for the ‘body to digest’ other foods, bowel movement and for prevention against certain diseases.
carbohydrates in the body.
Ans. Carbohydrates are widely distributed in plant foods. They are mainly present
in these foods in the form of three types of compounds called sugars, starches and
fiber.
as available and non-available carbohydrates. Carbohydrates like sugars and
starches are digestible in the human digestive tract and hence can be made available
to the body for its functioning. These carbohydrates are termed as available
carbohydrates. Fiber refers to a number of indigestible carbohydrates like cellulose
present in plant foods. cannot be digested in the human digestive tract and ate
non-available carbohydrates.
breakdown of starch and sugars like common table sugar in the diet to their simplest
unit namely, glucose. Dietary fiber present in whole grains, vegetables and fruits
cannot be digested by human beings because the stomach and intestines do not have
the necessary enzymes to do this job.
which is capable of breaking cooked starch into smaller units. However, the time
available for this enzyme to breakdown the starch in the mouth is too short to allow
for any significant amount of conversion to take place. The longer one chews the
food, the more the digestion of starch. There are no carbohydrate-digesting enzymes
in the stomach. Thus the principal site of carbohydrate digestion is the small
intestine. The major carbohydrate digesting enzyme present here is secreted by the
pancreas. This enzyme is capable of acting on both raw and cooked starch and
converts it into smaller units. The next phase of carbohydrate digestion takes place
within the cells of the small intestine. Enzymes present in the small intestine act on
sugars and partially digested starch and ultimately break them up into the simple
basic units i.e. glucose, fructose and galactose.
bloodstream and are ultimately converted to glucose. Some amount of glucose
remains in the blood as blood sugar and is drawn upon by the cells whenever
needed. In the body cells glucose is mainly burnt to release energy.
called glycogen which is subsequently stored in the liver and muscles. Glycogen can
be broken down to release glucose whenever needed. But only a limited amount of
glucose can be stored in the body as glycogen. Once the limit of glycogen storage is
exceeded, the remaining excess glucose is converted into fat and is stored in the
body.
Ans. Vitamin A
(1) Maintaining normal vision: Vitamin A plays an important role in maintaining
normal vision. To understand this better, we must first be familiar with the structure
of the eye. The retina has two kinds of cells – rods and cones. Both rods and cones
are sensitive to changes in light but they react differently and perform different
functions. While rods are sensitive to dim light, the cones respond to bright light.
Let us take a closer look at the rods. The rods contain a pigment called rhodopsin.
Rhodopsin is formed by the combination of a specific form of vitamin A with a
protein. The amazing thing about rhodopsin is that it breaks down into its
components when exposed to bright light. In the dark these components – vitamin A
and protein – again combine to regenerate rhodopsin.

(2) Supporting growth: Vitamin A is essential for the growth of the skeleton and soft
tissues. The exact role of the vitamin in the growth of the body is still not
understood. Research studies in this area have indicated that with the deficiency of
vitamin A in the body, bones do not grow to their full length and the overall growth
of the body is affected.
(3) Protecting against disease: Vitamin A plays an important role in keeping
epithelial tissues moist and healthy. Some examples of epithelial tissues are the skin,
the lining of our eyes and the lining of organs like the intestine and lungs. Without
vitamin A the epithelial tissue will become dry and cracks will appear in the skin or
inner walls of the digestive tract or lungs. This makes it easy for the germs to enter
and cause diseases like diarrhea, respiratory infections and eye infections. Various
research studies have supported this and shown that vitamin A plays a beneficial
role in preventing common illnesses in young children. When body levels of vitamin
A are low, the chances are more that the young child will develop, infectious
diseases. If these diseases are sufficiently severe they can even cause death.
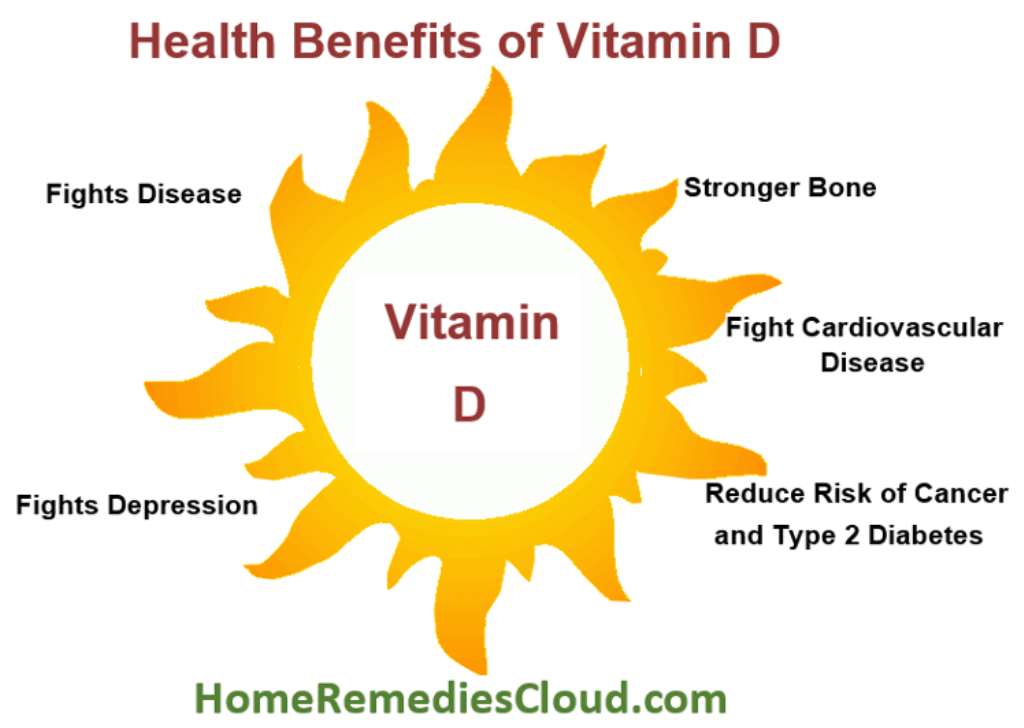
Vitamin D:
This is absolutely correct. How does vitamin D help in this? Read on to find out.
Minerals like calcium and phosphorus, when deposited in the bones, make them
strong and hard.
bones. Vitamin D aids the process of mineralization in two ways:
(i) by increasing the absorption of calcium and phosphorus and
(ii) by helping in the deposition of calcium and phosphorus in bones
Vitamin E:
substances like certain fatty acids, vitamins A and C. It prevents their destruction in
the body as well as in foods.

Vitamin K:
finger, of course, starts bleeding, but after a while blood stops oozing out. Why? This
is because a clot is formed on the wound and seals it off. Vitamin K plays an
important role in clotting of blood and is therefore also termed as the “antibleeding
vitamin” (one which prevents uncontrolled bleeding). How does vitamin K help in
clotting of blood?
It helps in the formation of a protein called prothrombin which, in turn, is essential
for blood clotting.

Ans.

(1) Development of bones and teeth:
- Calcium and phosphorus are mainly present in bones and teeth.
- The ratio of calcium and phosphorus in the bones is roughly 2:1
- Calcium in the bone combines with phosphorus, some other minerals and water to
form a compound. - It is this compound which provides rigidity and firmness to the
bones. - Teeth, like the bones, also require calcium for their proper development. It is
for this reason that the need for calcium is the most during the growing years.
(2) Regulation of body processes:
Apart from building bones and teeth, calcium and
phosphorus perform regulatory functions as well.
Calcium helps in:
(a) regulating the contraction and relaxation of muscles especially that of the heart
(b) regulating the passage of substances into and out of the cells
(c) conveying messages from one nerve cell to another and
(d) the clotting of blood.
Phosphorus also performs several important functions.
It is required for the:
(a) formation of a substance which aids in transport of fat in the blood
(b) synthesis of certain substances which promote the action of enzymes which play
a crucial role in metabolism

(a) Regulating the balance of extracellular and intracellular fluid:
- Sodium, the principal mineral in the extracellular fluid
- It is responsible for maintaining the fluid balance.
- By fluid balance we mean the process of maintaining a balance between the
fluid present within the cells (intracellular) and that circulating outside the cells
(extracellular). - Sodium along with potassium (another mineral) helps to maintain
this balance.
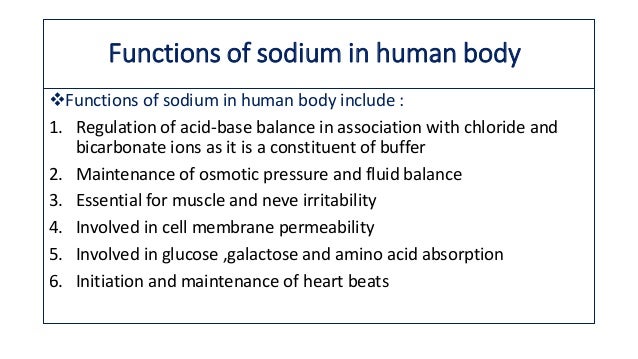
(b) Regulating the alkalinity and acidity of the body fluids:
- Sodium tends to make the body fluids alkaline
- Another mineral namely chloride present in the body fluids
tends to make them acidic - Sodium combines with chloride in the fluid and together
they help maintain the balance between the alkalinity and acidity of the body fluids.
(c) Aiding in the passage of messages from one nerve cell to another.
(d) Aiding the contraction of muscles
(e) Regulating the passage of substances into and out of the Cell.
Potassium
Functions: The functions of potassium include:
(a) Regulation of the balance of intracellular and extracellular fluid:
- Potassium along with sodium helps maintain fluid balance within the cell and outside the cell.
- Sodium is the main mineral present in extracellular fluid (the fluid outside the cell).
Potassium, on the other hand, is the principal mineral in the intracellular fluid.
Together these two minerals help maintain fluid balance.
(b) Regulation of the alkalinity/acidity of body fluids:
- Potassium, like sodium, is alkaline.
- It combines with chloride which is acidic and together they help maintain
the acidity/alkalinity of body fluids. - Sodium also has this function as you studied earlier
(c) Role in muscle activity:
- Potassium has a significant role in the activity of skeletal
and heart muscle. - It helps in the transmission of messages which results in the
contraction of muscle tissue.
Chloride
Functions:
- The functions of sodium, potassium and chloride are closely interlinked
as is evident from our earlier discussion. - Chloride combines with sodium and
potassium and helps regulate fluid balance and acidity/alkalinity of body fluids.
Functions: Magnesium helps in:
(a) regulating the passage of substances into and out of the calls
(b) maintaining the activity of many enzymes. Magnesium functions as a coenzyme
in metabolism
(C) building bones and teeth. It is involved in bone mineralization
(d) maintaining the functions of the nervous system, whereby it helps in the passage
of messages from one nerve cell to another
(e) maintaining smooth muscle action and
(f) building proteins.
Functions: After many years of research, there are still many puzzling aspects about
the role of iron, especially about those related to brain functioning. Let us now study
some of the known and well established functions of iron.
/iron-supplements-benefits-4178814-5c4e40cd46e0fb00014c370c.png)
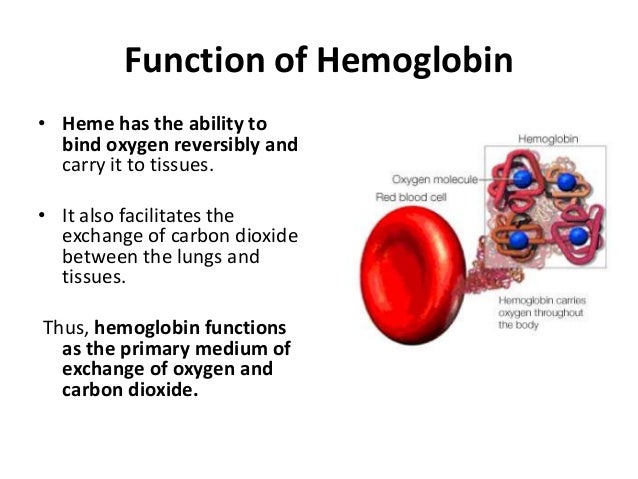
(a) Oxygen transport:
- Iron is a major constituent of a red-colored compound called
hemoglobin present in the blood. - What is the role of hemoglobin? Hemoglobin is
necessary for transport of oxygen to various parts of the body. - Hemoglobin carries oxygen from the lungs to the tissues.
- It then helps in carrying carbon dioxide from
the tissues to the lungs. From the lungs carbon dioxide is
then exhaled out. - Carbon dioxide, in fact, is a waste product formed in all cells as a
result of metabolism and it needs to be removed from the body.
(b) Provision of oxygen for muscle contraction:
- Iron is also present in the muscle in
the form of a substance which has the capacity to store oxygen. - This oxygen is used for muscle contraction and for other immediate needs of the muscle cells.
(c) Promotion of oxidation within cells:
- When carbohydrates, proteins and fats are
broken down in body cells, energy is released. - Iron helps in complete breakdown of
these nutrients. - You know that energy is required for the various physical activities
we perform every day. - This is the reason why iron is crucial in helping us to perform
physical work.
Iodine
Functions:
- Why do we need iodine? Iodine is a component of the hormone thyroxine
secreted by the thyroid gland. - Thyroxine regulates the rate at which chemical
reactions take place in the body cells. - If this regulation does not take place, both
physical and mental growth will be affected. - Iodine is also believed to help in the
functioning of nerve and muscle tissues.

Ans. Calcium and Phosphorus
Food sources:
- Which foods provide good amounts of calcium? Milk and milk
products like curd, channa cottage cheese) are excellent sources of calcium. - Foods like fish especially dried fish and other sea foods (e.g. crab) provide substantial quantities of calcium.

- Among the plant sources, ragi (a millet grown in South India) is particularly rich in
calcium. - Pulses like bengal gram, black gram, green gram, moth beans, rajmah,
soyabean contribute substantial amounts of calcium. - Green leafy vegetables (like
amaranth leaves, colocasia leaves, fenugreek leaves, mustard leaves) also contain
good amounts. Among nuts and oilseeds, gingelly (til) seed is particularly rich in
calcium.
Sodium
Food sources:
- Do you know what items in our diet provide maximum sodium? You
are familiar with common table salt which is nothing but sodium chloride. - Common table salt is the principal source of sodium in our diet.
- One teaspoon of salt provides almost 2000 mg sodium.
- Other rich sources of sodium include milk, egg white, meat,
poultry, fish among the animal foods and green leafy vegetables (such as spinach,
fenugreek leaves) and pulses among the plant sourcesSodium losses are highwhenever we sweat more as in hot weather. Any disease condition in which water is lost from the body also causes excessive sodium loss.
- A common example is diarrhea i.e. loose motions. Excessive sodium loss is not good as
it affects the fluid balance of the body. This requires special attention. Intake of fluids
and salt should be increased during such times so as to make up for the loss.
Potassium
Food sources: Potassium is widely distributed in foods. Meat, poultry and fish are
good sources. Among the plant foods, pulses, fruits, vegetables especially the green
leafy vegetables are good sources of potassium. The water of the tender coconut is,
however, the best source of potassium. Among the other fruits and vegetables.
bananas, potatoes, carrots, tomatoes and lemons contain appreciable amounts of this
mineral. Whole grain cereals also provide some amounts of potassium.
Food sources:
important source of chloride in our diet is common table salt ‘ie, sodium chloride.
Sources:
widely distributed in plant foods. The most concentrated sources of magnesium
include nuts (groundnut, cashewnut, walnut, almond), oilseeds (sesame seeds).
pulses (rajmah, moth beans, soybean), whole grains (wheat, bajra, jowar). Among
sea foods shellfish is particularly rich in magnesium. Other foods which contain
appreciable amounts of magnesium include dark green leafy vegetables, peas, lotus
stem, fish (salmon, haddock), sea foods (crab, oyster) and meat.
Liver is an excellent source. Other organ meats like kidney, spleen also contain
substantial amounts of iron. Among the plant foods the list of iron sources includes
green leafy vegetables (like’ amaranth leaves, mustard leaves, colocasia leaves, mint
leaves), cereals (like whole wheat flour, rice flakes, bajra, ragi, jowar) and pulses
(especially the whole ones). Soybean is an example of a pulse containing good
amounts of iron. Jaggery is another food that contains fair amounts of iron.
We have mentioned several foods which contain substantial amounts of iron.
However, we have a paradoxical situation here. There is so much of iron present in
food and yet very little gets into the body.
iodine content of sol1 and water. Crops such as vegetables especially those grown in
coastal areas where iodine content of the soil is high have substantial amounts of
iodine. In hilly areas, however, the iodine content of both the soil and water is low.
Hence the crops grown in such areas contain little iodine.
The iodine content of animal foods like eggs, dairy products and meat depends, of
course, on the iodine content of the food that is part of the animal’s diet. Sea foods
like fish, shell fish are among the best sources of iodine.
Lactation.(10 MARK)
Ans. Due to the rapid growth in the foetal tissues(ଭ୍ରୁଣ ଟିସୁ )and maternal tissues(ମାତୃ ଟିସୁ ), basal
metabolic rate or BMR also goes up.

reactions going on inside the body cells proceed at a faster pace. The word “basal”
refers to the state of the normal body when at complete rest but not sleeping Basal
metabolic rate is best measured early in the morning when the person has just
woken up. The increase in basal metabolic rate or BMR is one of the reasons why
energy requirements go up sharply from the second trimester of pregnancy.
(i) that growth itself is a process requiring high levels of energy, and
(ii) that energy is stored in the body in the form of fat.
Now, you are aware that protein is required for body-building. So, in a high growth
phase like pregnancy, what would happen to protein needs? Yes, they would go up
sharply in order to sustain the process of rapid-growth of both foetus and maternal
tissues. The growth of both foetal and maternal tissues becomes substantial from the
second trimester onwards.
from the second trimester. B vitamins such
as thiamine, riboflavin and niacin form part of coenzymes involved in helping to
release the energy locked into molecules of carbohydrate or fat.
is a little different. Coenzymes synthesized from folic acid play an important role in
the process of cell multiplication which, as you know, is part of the process of
growth. Hence folic acid requirements go up sharply for this reason.
Requirements for iron and calcium also go up substantially from the second
trimester onwards. Iron is needed for synthesis of hemoglobin. This forms a part of
the several new red blood cells
formed in the mother’s bloodstream as well as in that
of the foetus.
the first three to four months of life after birth. This further raises the iron
requirement. Calcium is deposited in large amounts in the bones of the developing
foetus. This is the reason why calcium needs go up in pregnancy.
Iodine by the mother? Iodine deficiency results in cretinism – a condition associated
deafness. Intake of adequate iodine by the pregnant woman is therefore crucial to
ensure proper regulation of physical and mental development of the foetus.
the second trimester onwards. Can you think of a reason for this? The reason is that
in the first trimester (0-3 months) the foetus is small and its nutritional needs are not
significant. The associated changes in the organs and tissues of the mother also
remain insignificant
development of the foetus are met by the mother’s diet.
essential amounts, the mother’s own tissues would be broken down. You can
imagine the effect on the health of an already malnourished woman in pregnancy if
she does not consume a proper diet!

nutritional status. The diet of the girl during adolescence is crucial in preparing the
body for pregnancy. However, many of the adolescent girls in our country do not
get a chance to complete their growth and they remain
undernourished. In fact,
imposes a heavy strain on the girl, pushing up nutrient needs very high. She faces
the burden of meeting the increased nutrient needs required for supporting her own
rapid growth in adolescence as well as the increased nutrient needs imposed by
pregnancy. Very often these increased needs cannot be met. The result? The girl may
become severely malnourished and the baby is born too small. Neither mother nor
infant may survive. We will discuss the heavy price of malnutrition in greater detail
in Several studies have shown that a well- nourished woman with adequate nutrient
reserves is better equipped for a successful pregnancy. In other words diet before
pregnancy is important so that nutrient reserves or stores are available in the body.
However, this must be followed up with a good diet during pregnancy to prevent
the mother and infant becoming malnourished.
Ans. Some complications which can occur in the newborn are as follows:
Umbilical Infection: Umbilical infection may occur in the case of unsterile cord if
cutting. Purulent discharge red and inflamed periumbilical area and foul smell are
indicative of umbilical sepsis. The doctor must be consulted in this case.
ଅମ୍ବିଲିକ୍ ସଂକ୍ରମଣ: ଅସ୍ଥିର କର୍ଡ କ୍ଷେତ୍ରରେ ନାବିକ ସଂକ୍ରମଣ ହୋଇପାରେ |
କାଟିବା ଶୁଦ୍ଧ ନିଷ୍କାସନ ଲାଲ ଏବଂ ପ୍ରଦାହିତ ପେରିମ୍ବିଲିକାଲ୍ କ୍ଷେତ୍ର ଏବଂ ଦୁର୍ଗନ୍ଧ |
ନାବିକ ସେପସିସ୍ ର ସୂଚକ | ଏହି କ୍ଷେତ୍ରରେ ଡାକ୍ତରଙ୍କ ପରାମର୍ଶ ନେବା ଜରୁରୀ )
Umbilical Infection: Umbilical Infection हो सकता है अगर unsterile cord के मामले में
काट रहा है। पुरुलेंट डिस्चार्ज लाल और सूजन वाले पेरिम्बिलिकल क्षेत्र और फाउल गंध हैं
नाभि सेप्सिस का संकेत। इस मामले में डॉक्टर से परामर्श किया जाना चाहिए।)

Eye Infection: Eye infection may be caused by some germs transmitted from the
genital tract during delivery or by infected hands of caregivers. Profuse purulent
discharge may occur in one or both the eyes. The doctor should be consulted. Sticky
eyes without purulent discharge are common during first 2-3 days after birth and are
not a cause for alarm. In such a case, the eyes should be cleaned daily with sterile
ପ୍ରସବ ସମୟରେ କିମ୍ବା ଯତ୍ନ ନେଉଥିବା ବ୍ୟକ୍ତିଙ୍କ ଦ୍ gen ାରା ଯ ital ନାଙ୍ଗ ଟ୍ରାକ୍ଟ | ପ୍ରଫୁଲ୍ଲ
ଗୋଟିଏ କିମ୍ବା ଉଭୟ ଆଖିରେ ଡିସଚାର୍ଜ ହୋଇପାରେ | ଡାକ୍ତରଙ୍କ ପରାମର୍ଶ ନେବା ଉଚିତ୍। ଷ୍ଟିକି |
ଶୁଦ୍ଧ ନିଷ୍କାସନ ବିନା ଆଖି ଜନ୍ମ ହେବାର ପ୍ରଥମ 2-3 ଦିନ ମଧ୍ୟରେ ସାଧାରଣ ଅଟେ ଏବଂ |
ଆଲାର୍ମର କାରଣ ନୁହେଁ | ଏପରି ପରିସ୍ଥିତିରେ, ଆଖିକୁ ପ୍ରତିଦିନ ଷ୍ଟେରାଇଲ୍ ସହିତ ସଫା କରାଯିବା ଉଚିତ୍ |
ପ୍ରତ୍ୟେକ ଆଖି ପାଇଁ ଗୋଟିଏ ସ୍ୱାବ ବ୍ୟବହାର କରି ସାଧାରଣ ସି iled ା ପାଣିରେ ଭିଜାଯାଇଥିବା ସୂତା ସ୍ ab ାବ୍ |
ନିର୍ଦ୍ଦିଷ୍ଟ ଆଖି ବୁନ୍ଦା ବ୍ୟବହାର କରାଯାଇପାରେ |)
प्रसव के दौरान या देखभाल करने वालों के संक्रमित हाथों से जननांग पथ। विपुल प्रयोजन
एक या दोनों आंखों में डिस्चार्ज हो सकता है। डॉक्टर से परामर्श किया जाना चाहिए। चिपचिपा
प्यूरुलेंट डिस्चार्ज के बिना आँखें जन्म के बाद पहले 2-3 दिनों के दौरान आम हैं और हैं
अलार्म का कारण नहीं। ऐसे मामले में, बाँझ के साथ आंखों को रोजाना साफ किया जाना चाहिए
कपास झाड़ू प्रत्येक आंख के लिए एक झाड़ू का उपयोग करके सामान्य उबले पानी में भिगोया जाता है।
निर्धारित आई ड्रॉप का उपयोग किया जा सकता है।)

Weight loss: Most babies lose weight during the first 2-3 days of life. The weight loss
usually varies between 5 and 8 per cent of birth weight The normal factors
contributing to initial weight loss include removal of vernix, mucus and blood from
skin, passage of meconium and reduction of extra-cellular fluid volume. Nonnal
birth weight is regained by the end of first week. But weight loss may be excessive
due to:
– lack of oral feeding
– delayed feeding
– persistent vomiting
– diarrhea
– Mother taking certain drugs
– cleft lip and crert palate
In this regard, the following measures are recommended:
Accurate weighing of babies. Weight should be routinely recorded. Mother should
be advised to put the baby to breast frequently so that lactation is adequate.”
Intravenous feeding may be recommended for babies in case weight loss is serious.
ସାଧାରଣତ birth ଜନ୍ମ ଓଜନର 5 ରୁ 8 ପ୍ରତିଶତ ମଧ୍ୟରେ ଭିନ୍ନ ହୋଇଥାଏ ସାଧାରଣ କାରଣଗୁଡିକ |
ପ୍ରାରମ୍ଭିକ ଓଜନ ହ୍ରାସ କରିବାରେ ଭର୍ନିକ୍ସ, ମକୁସ୍ ଏବଂ ରକ୍ତ ଅପସାରଣ ଅନ୍ତର୍ଭୁକ୍ତ |
ଚର୍ମ, ମେକୋନିୟମର ଗତି ଏବଂ ଅତିରିକ୍ତ ସେଲ୍ୟୁଲାର୍ ଫ୍ଲୁଇଡ୍ ପରିମାଣ ହ୍ରାସ | ଅଣନାଲ୍ |
ପ୍ରଥମ ସପ୍ତାହ ଶେଷ ସୁଦ୍ଧା ଜନ୍ମ ଓଜନ ପୁନ ained ପ୍ରାପ୍ତ ହୁଏ | କିନ୍ତୁ ଓଜନ ହ୍ରାସ ହୋଇପାରେ |
କାରଣରୁ:
– ମ oral ଖିକ ଖାଇବାକୁ ଅଭାବ |
– ଖାଇବାକୁ ଦେବାରେ ବିଳମ୍ବ |
– କ୍ରମାଗତ ବାନ୍ତି |
– ଡାଇରିଆ
– ମା କିଛି drugs ଷଧ ସେବନ କରନ୍ତି |
– କ୍ଲିପ୍ ଲିପ୍ ଏବଂ କ୍ରେଟ୍ ପ୍ୟାଲେଟ୍ |
ଏହି ପରିପ୍ରେକ୍ଷୀରେ, ନିମ୍ନଲିଖିତ ପଦକ୍ଷେପଗୁଡିକ ସୁପାରିଶ କରାଯାଇଛି:
ଶିଶୁମାନଙ୍କର ସଠିକ୍ ଓଜନ | ଓଜନ ନିୟମିତ ଭାବରେ ରେକର୍ଡ କରାଯିବା ଉଚିତ୍ | ମାତା କରିବା ଉଚିତ୍ |
ଶିଶୁକୁ ବାରମ୍ବାର ସ୍ତନ୍ୟପାନ କରାଇବାକୁ ପରାମର୍ଶ ଦିଅନ୍ତୁ ଯାହାଦ୍ୱାରା ସ୍ତନ୍ୟପାନ ଯଥେଷ୍ଟ ହେବ | “
ଓଜନ ହ୍ରାସ ଗୁରୁତର ହେଲେ ଶିଶୁମାନଙ୍କ ପାଇଁ ଶିରାଭ୍ୟନ୍ତର ଖାଇବାକୁ ସୁପାରିଶ କରାଯାଇପାରେ |)
आमतौर पर जन्म के वजन के 5 और 8 प्रतिशत के बीच भिन्न होता है सामान्य कारक
प्रारंभिक वजन घटाने में योगदान से वर्निक्स, बलगम और रक्त को निकालना शामिल है
त्वचा, मेकोनियम का पारित होना और अतिरिक्त कोशिकीय द्रव की मात्रा में कमी। Nonnal
जन्म का वजन पहले सप्ताह के अंत तक प्राप्त होता है। लेकिन वजन घटाना अत्यधिक हो सकता है
की वजह से:
– ओरल फीडिंग की कमी
– दूध पिलाने में देरी
– लगातार उल्टी होना
– दस्त
– कुछ दवाएं लेने वाली माँ
– फांक होंठ और कश तालु
इस संबंध में, निम्नलिखित उपायों की सिफारिश की जाती है:
शिशुओं का सटीक वजन। वजन नियमित रूप से दर्ज किया जाना चाहिए। माँ चाहिए
बच्चे को बार-बार स्तनपान कराने की सलाह दी जाए ताकि स्तनपान पर्याप्त हो। ”
वजन कम होने की स्थिति में शिशुओं के लिए अंतःशिरा भक्षण की सिफारिश की जा सकती है।

Oral Thrush: This infection generally occurs during the newborn period. White
patches or spots appear over the tongue, palate and gums. The baby may not be able
to suck normally. In such a case, the mother should be advised to administer or
apply prescribed medications and maintain hygiene.
ଜିଭ, ପାଲଟ୍ ଏବଂ ଗୁଣ୍ଡ ଉପରେ ପ୍ୟାଚ୍ କିମ୍ବା ଦାଗ ଦେଖାଯାଏ | ଶିଶୁଟି ସକ୍ଷମ ହୋଇନପାରେ |
ସାଧାରଣ ଭାବରେ ଶୋଷିବାକୁ | ଏପରି ପରିସ୍ଥିତିରେ, ମାତାଙ୍କୁ ପରିଚାଳନା କରିବାକୁ ପରାମର୍ଶ ଦେବା ଉଚିତ୍ କିମ୍ବା
ନିର୍ଦ୍ଦିଷ୍ଟ ications ଷଧ ପ୍ରୟୋଗ କରନ୍ତୁ ଏବଂ ସ୍ୱଚ୍ଛତା ବଜାୟ ରଖନ୍ତୁ |)
पैच या स्पॉट जीभ, तालु और मसूड़ों के ऊपर दिखाई देते हैं। बच्चा सक्षम नहीं हो सकता है
सामान्य रूप से चूसना। ऐसे मामले में, माँ को प्रशासन या करने की सलाह दी जानी चाहिए
निर्धारित दवाएं लागू करें और स्वच्छता बनाए रखें।

DECE2-Solution(ENG/HIN)(CH-3)-IGNOU-DAY 14-ORSP
Ans. “Antenatal Care” is the care given to the woman during pregnancy. It consists
of early detection and confirmation of pregnancy, detection of ‘at risk’ mother,
immunization against tetanus, nutritional supplementation with iron and folic acid
and periodic antenatal assessment. Antenatal assessment, to be made at least at 20,
30, 34 and 38 weeks of pregnancy, also aims at early detection of foetal growth
failure.

ଗର୍ଭଧାରଣର ଶୀଘ୍ର ଚିହ୍ନଟ ଏବଂ ନିଶ୍ଚିତକରଣ, ‘ବିପଦରେ’ ମା’ର ଚିହ୍ନଟ,
ଟିଟାନସ୍ ପ୍ରତି ପ୍ରତିରୋପଣ, ଲୁହା ଏବଂ ଫୋଲିକ୍ ଏସିଡ୍ ସହିତ ପୁଷ୍ଟିକର ସପ୍ଲିମେଣ୍ଟେସନ୍ |
ଏବଂ ପର୍ଯ୍ୟାୟକ୍ରମେ ପ୍ରସବକାଳୀନ ମୂଲ୍ୟାଙ୍କନ | ଅନ୍ତତ at ପକ୍ଷେ ମୂଲ୍ୟାଙ୍କନ, ଅତିକମରେ 20,
ଗର୍ଭଧାରଣର 30, 34 ଏବଂ 38 ସପ୍ତାହ, ଗର୍ଭସ୍ଥ ବୃଦ୍ଧିର ଶୀଘ୍ର ଚିହ୍ନଟ କରିବାକୁ ମଧ୍ୟ ଲକ୍ଷ୍ୟ ରଖିଛି |
ବିଫଳତା)
गर्भावस्था का प्रारंभिक पता लगाने और पुष्टि करने के लिए, ‘जोखिम में’ मां का पता लगाने,
टेटनस के खिलाफ टीकाकरण, लोहे और फोलिक एसिड के साथ पोषण पूरकता
और समय-समय पर प्रसवपूर्व मूल्यांकन। प्रसव के बाद मूल्यांकन, कम से कम 20 पर किया जाना है,
गर्भावस्था के 30, 34 और 38 सप्ताह, भी भ्रूण के विकास का जल्द पता लगाने के लिए लक्ष्य रखते हैं
विफलता।
medical doctor. The pregnant woman is entitled to the highest standard of care
during this period and needs to have faith in the health team, for the safety and care
of her baby and herself. Proper antenatal care provides adequate medical,
nutritional, physical, psychological, social and educational care to the pregnant
woman. Before we go into the details of antenatal care, let us see what it aims at.
The aims of antenatal care are to promote and maintain good physical and mental
health of the pregnant woman ensure the birth of a mature, live and healthy child to
a healthy mother prepare the woman for labor and delivery detect early and treat
any high risk conditions endangering the life of the mother and child teach the
woman about family planning and care of the newborn.
ଡାକ୍ତରୀ ଡାକ୍ତର। ଗର୍ଭବତୀ ମହିଳା ସର୍ବୋଚ୍ଚ ଯତ୍ନର ଅଧିକାର ପାଇଛନ୍ତି
ଏହି ଅବଧି ମଧ୍ୟରେ ଏବଂ ନିରାପତ୍ତା ଏବଂ ଯତ୍ନ ପାଇଁ ସ୍ୱାସ୍ଥ୍ୟ ଦଳ ଉପରେ ବିଶ୍ୱାସ ରହିବା ଆବଶ୍ୟକ |
ତା’ର ଶିଶୁ ଏବଂ ନିଜେ | ସଠିକ୍ ପ୍ରସବ ଯତ୍ନ ପର୍ଯ୍ୟାପ୍ତ ଚିକିତ୍ସା ଯୋଗାଏ,
ଗର୍ଭବତୀଙ୍କୁ ପୁଷ୍ଟିକର, ଶାରୀରିକ, ମାନସିକ, ସାମାଜିକ ଏବଂ ଶିକ୍ଷାଗତ ଯତ୍ନ |
ମହିଳା ପ୍ରସବକାଳୀନ ଯତ୍ନର ସବିଶେଷ ତଥ୍ୟକୁ ଯିବା ପୂର୍ବରୁ, ଆସନ୍ତୁ ଦେଖିବା ଏହାର ଉଦ୍ଦେଶ୍ୟ କ’ଣ
ପ୍ରସବକାଳୀନ ଯତ୍ନର ଉଦ୍ଦେଶ୍ୟ ହେଉଛି ଉତ୍ତମ ଶାରୀରିକ ଏବଂ ମାନସିକତାକୁ ପ୍ରୋତ୍ସାହନ ଏବଂ ପରିଚାଳନା କରିବା |
ଗର୍ଭବତୀ ମହିଳାଙ୍କ ସ୍ୱାସ୍ଥ୍ୟ ଏକ ପରିପକ୍ୱ, ଜୀବନ୍ତ ଏବଂ ସୁସ୍ଥ ସନ୍ତାନର ଜନ୍ମ ନିଶ୍ଚିତ କରେ |
ଜଣେ ସୁସ୍ଥ ମାତା ମହିଳାଙ୍କୁ ଶ୍ରମ ଏବଂ ପ୍ରସବ ପାଇଁ ଶୀଘ୍ର ଚିହ୍ନଟ କରି ଚିକିତ୍ସା ପାଇଁ ପ୍ରସ୍ତୁତ କରନ୍ତି |
ମା ଏବଂ ଶିଶୁର ଜୀବନ ପ୍ରତି ବିପଦ ଥିବା ଯେକ high ଣସି ଉଚ୍ଚ ବିପଦ ଅବସ୍ଥା ଶିକ୍ଷା ଦିଏ |
ପରିବାର ଯୋଜନା ଏବଂ ନବଜାତ ଶିଶୁର ଯତ୍ନ ବିଷୟରେ ମହିଳା |
चिकित्सा चिकित्सक। गर्भवती महिला देखभाल के उच्चतम मानक की हकदार है
इस अवधि के दौरान और सुरक्षा और देखभाल के लिए स्वास्थ्य टीम में विश्वास रखने की जरूरत है
उसके बच्चे और खुद के। उचित प्रसव पूर्व देखभाल पर्याप्त चिकित्सा प्रदान करती है,
गर्भवती को पोषण, शारीरिक, मनोवैज्ञानिक, सामाजिक और शैक्षिक देखभाल
महिला। इससे पहले कि हम प्रसवपूर्व देखभाल के विवरण में जाएं, आइए देखें कि इसका उद्देश्य क्या है।
प्रसवपूर्व देखभाल के उद्देश्य अच्छे शारीरिक और मानसिक को बढ़ावा देना और बनाए रखना है
गर्भवती महिला का स्वास्थ्य परिपक्व, जीवित और स्वस्थ बच्चे के जन्म को सुनिश्चित करता है
एक स्वस्थ माँ महिला को प्रसव और प्रसव के लिए तैयार करती है और जल्दी पता लगा लेती है
मां और बच्चे के जीवन को खतरे में डालने वाली कोई भी उच्च जोखिम वाली स्थिति
परिवार नियोजन और नवजात शिशु की देखभाल के बारे में महिला।

Ans. As you have read, good health is defined as the physical, intellectual and
psychological well-being of the person. A healthy child is one who can cope with het
environment in a manner appropriate for her age group, and, therefore, displays
physical, mental and emotional balance. When such a balance is disturbed by illness,
it affects all aspects of the child’s life-physical, cognitive, emotional and social
You may have noticed that it is usually the mother who first recognizes that
something is wrong with her child, even before specific symptoms of an illness
appear. This is because the mother deals with her child as a complete being, and is
conscious of disturbance in the whole. Development of a child is not only affected by
many factors (cultural, economic, social or even accidental), it is also multi-
dimensional (proceeding. in more than one area or facet) and integrated (each area
affecting the others) and takes place continuously. Therefore, our concern when
talking of providing health care to the child should not just be ensuring that the child
survives, by providing physical care.
child develop as a total being. Survival and development
Rather, we have to help
have to proceed together. We are not dealing with a sequential process, wherein we
inseparable
Therefore, care of either healthy or sick children must equally take a holistic
approach, viewing the entire human being as its concern. It is not adequate to treat
the physical symptoms of the illness. It is crucial to care for the whole child –
looking after her emotional, social and stimulation seeds, along with providing
physical care. We, therefore, advocate a multidimensional approach to child care, in
health and in sickness.
ବ୍ୟକ୍ତିର ମାନସିକ ସୁସ୍ଥତା | ଏକ ସୁସ୍ଥ ଶିଶୁ ହେଉଛି ଯିଏ ହେଟ୍ ସହିତ ମୁକାବିଲା କରିପାରିବ |
ତାଙ୍କ ବୟସ ଶ୍ରେଣୀ ପାଇଁ ଉପଯୁକ୍ତ manner ଙ୍ଗରେ ପରିବେଶ, ଏବଂ, ତେଣୁ, ପ୍ରଦର୍ଶନ କରେ |
ଶାରୀରିକ, ମାନସିକ ଏବଂ ଭାବନାତ୍ମକ ସନ୍ତୁଳନ | ଯେତେବେଳେ ଅସୁସ୍ଥତା ଦ୍ୱାରା ଏପରି ସନ୍ତୁଳନ ବିଚଳିତ ହୁଏ,
ଏହା ଶିଶୁର ଜୀବନ-ଶାରୀରିକ, ଜ୍ଞାନଗତ, ଭାବପ୍ରବଣ ଏବଂ ସାମାଜିକର ସମସ୍ତ ଦିଗକୁ ପ୍ରଭାବିତ କରିଥାଏ |
ଆପଣ ହୁଏତ ଧ୍ୟାନ ଦେଇଥିବେ ଯେ ସାଧାରଣତ the ସେହି ମା ହିଁ ପ୍ରଥମେ ଏହାକୁ ଚିହ୍ନିଥାଏ |
ରୋଗର ନିର୍ଦ୍ଦିଷ୍ଟ ଲକ୍ଷଣ ପୂର୍ବରୁ ମଧ୍ୟ ତାଙ୍କ ପିଲାଙ୍କ ସହିତ କିଛି ଭୁଲ ଅଛି |
ଦେଖାଯାଏ | ଏହାର କାରଣ ହେଉଛି, ମା ନିଜ ସନ୍ତାନ ସହିତ ସଂପୂର୍ଣ୍ଣ ସୃଷ୍ଟିକର୍ତ୍ତା ଭାବରେ କାର୍ଯ୍ୟ କରେ, ଏବଂ ଅଟେ |
ସମଗ୍ର ବିଶୃଙ୍ଖଳା ବିଷୟରେ ସଚେତନ | ଏକ ଶିଶୁର ବିକାଶ କେବଳ ପ୍ରଭାବିତ ହୁଏ ନାହିଁ |
ଅନେକ କାରଣ (ସାଂସ୍କୃତିକ, ଅର୍ଥନ, ତିକ, ସାମାଜିକ କିମ୍ବା ଏପରିକି ଦୁର୍ଘଟଣାଜନକ), ଏହା ମଧ୍ୟ ବହୁ-
ଡାଇମେନ୍ସନାଲ୍ (ଅଗ୍ରଗତି | ଏକରୁ ଅଧିକ କ୍ଷେତ୍ର କିମ୍ବା ଦିଗରେ) ଏବଂ ଏକୀକୃତ (ପ୍ରତ୍ୟେକ କ୍ଷେତ୍ର) |
ଅନ୍ୟମାନଙ୍କୁ ପ୍ରଭାବିତ କରେ) ଏବଂ କ୍ରମାଗତ ଭାବରେ ଘଟେ | ତେଣୁ, ଆମର ଚିନ୍ତା କେବେ |
ଶିଶୁକୁ ସ୍ୱାସ୍ଥ୍ୟ ସେବା ଯୋଗାଇବା ବିଷୟରେ କହିବା କେବଳ ଶିଶୁକୁ ନିଶ୍ଚିତ କରିବା ଉଚିତ୍ ନୁହେଁ |
ଶାରୀରିକ ଯତ୍ନ ଯୋଗାଇ ବଞ୍ଚିଥାଏ |
ଶିଶୁ ସମୁଦାୟ ଭାବରେ ବିକାଶ ହୁଏ | ବଞ୍ଚିବା ଏବଂ ବିକାଶ
ବରଂ ଆମକୁ ସାହାଯ୍ୟ କରିବାକୁ ପଡିବ |
ଏକତ୍ର ଅଗ୍ରଗତି କରିବାକୁ ପଡିବ | ଆମେ ଏକ କ୍ରମିକ ପ୍ରକ୍ରିୟା ସହିତ କାରବାର କରୁନାହୁଁ, ଯେଉଁଠାରେ ଆମେ |
ପିଲାକୁ ପ୍ରଥମେ ବଞ୍ଚିବାକୁ ଏବଂ ପରେ ବିକାଶରେ ସାହାଯ୍ୟ କର | ସ୍ୱାସ୍ଥ୍ୟ ଏବଂ ବିକାଶ ହେଉଛି |
ଅବିଚ୍ଛେଦ୍ୟ |
ତେଣୁ, ସୁସ୍ଥ କିମ୍ବା ଅସୁସ୍ଥ ପିଲାମାନଙ୍କର ଯତ୍ନ ସମାନ ଭାବରେ ଏକ ସାମଗ୍ରିକ ହେବା ଆବଶ୍ୟକ |
ଆଭିମୁଖ୍ୟ, ସମଗ୍ର ମଣିଷକୁ ଏହାର ଚିନ୍ତା ଭାବରେ ଦେଖିବା | ଚିକିତ୍ସା କରିବା ପର୍ଯ୍ୟାପ୍ତ ନୁହେଁ |
ରୋଗର ଶାରୀରିକ ଲକ୍ଷଣ | ସମଗ୍ର ଶିଶୁର ଯତ୍ନ ନେବା ଅତ୍ୟନ୍ତ ଗୁରୁତ୍ୱପୂର୍ଣ୍ଣ –
ଯୋଗାଇବା ସହିତ ତା’ର ଭାବପ୍ରବଣ, ସାମାଜିକ ଏବଂ ଉତ୍ସାହ ମଞ୍ଜିଗୁଡ଼ିକର ଯତ୍ନ ନେବା |
ଶାରୀରିକ ଯତ୍ନ ତେଣୁ, ଆମେ ଶିଶୁ ଯତ୍ନ ପାଇଁ ଏକ ବହୁମୁଖୀ ଆଭିମୁଖ୍ୟକୁ ପ୍ରୋତ୍ସାହିତ କରୁ |
ସ୍ୱାସ୍ଥ୍ୟ ଏବଂ ଅସୁସ୍ଥତା |
व्यक्ति का मनोवैज्ञानिक कल्याण। एक स्वस्थ बच्चा वह है जो हेट का सामना कर सकता है
उसके आयु समूह के लिए उपयुक्त वातावरण, और, इसलिए, प्रदर्शित करता है
शारीरिक, मानसिक और भावनात्मक संतुलन। जब ऐसा संतुलन बीमारी से परेशान है,
यह बच्चे के जीवन-भौतिक, संज्ञानात्मक, भावनात्मक और सामाजिक सभी पहलुओं को प्रभावित करता है
आपने देखा होगा कि यह आमतौर पर मां ही होती है जो सबसे पहले इसे पहचानती है
किसी बीमारी के विशिष्ट लक्षणों से पहले भी उसके बच्चे के साथ कुछ गलत है
दिखाई देते हैं। ऐसा इसलिए है क्योंकि माँ अपने बच्चे के साथ एक पूर्ण व्यवहार करती है, और है
पूरे में गड़बड़ी के प्रति सचेत। एक बच्चे का विकास न केवल प्रभावित होता है
कई कारक (सांस्कृतिक, आर्थिक, सामाजिक या आकस्मिक), यह भी बहु है-
आयामी (आगे बढ़ना। एक से अधिक क्षेत्र या पहलू में) और एकीकृत (प्रत्येक क्षेत्र
दूसरों को प्रभावित करना) और लगातार जगह लेता है। इसलिए, जब हमारी चिंता
बच्चे को स्वास्थ्य देखभाल प्रदान करने की बात सिर्फ यह सुनिश्चित करने की नहीं होनी चाहिए कि बच्चा
जीवित, शारीरिक देखभाल प्रदान करके।
बाल कुल के रूप में विकसित होते हैं। अस्तित्व और विकास
बल्कि हमें मदद करनी होगी
एक साथ आगे बढ़ना है। हम एक अनुक्रमिक प्रक्रिया के साथ काम नहीं कर रहे हैं, जिसमें हम
बच्चे को पहले जीवित रहने और फिर विकसित करने में मदद करें। स्वास्थ्य और विकास है
अवियोज्य
इसलिए, या तो स्वस्थ या बीमार बच्चों की देखभाल समान रूप से एक समग्र होनी चाहिए
दृष्टिकोण, संपूर्ण मानव को इसकी चिंता के रूप में देखना। यह इलाज के लिए पर्याप्त नहीं है
बीमारी के शारीरिक लक्षण। पूरे बच्चे की देखभाल करना महत्वपूर्ण है –
प्रदान करने के साथ उसके भावनात्मक, सामाजिक और उत्तेजना बीज की देखभाल करना
शारीरिक देखभाल। इसलिए, हम बच्चे की देखभाल में बहुआयामी दृष्टिकोण की वकालत करते हैं
स्वास्थ्य और बीमारी में।
Ans. An important part of health care is knowing the proper history of the child and
her environment. For this purpose, it would be helpful if you have a card for each
child in which you record the various aspects o the child’s health, as described in this
section. Alternatively, you could also use a register giving a few pages for each child.
This record would serve as a ready reference or you as well as the doctor/health
worker. Much of the information about the following aspects will be obtained from
the mother. You may talk to her during her visit to the center or you may need to
visit her at home.
ତା’ର ପରିବେଶ ଏହି ଉଦ୍ଦେଶ୍ୟ ପାଇଁ, ଯଦି ଆପଣଙ୍କର ପ୍ରତ୍ୟେକ ପାଇଁ କାର୍ଡ ଅଛି ତେବେ ଏହା ସହାୟକ ହେବ |
ଶିଶୁ ଯେଉଁଥିରେ ତୁମେ ଶିଶୁର ସ୍ୱାସ୍ଥ୍ୟର ବିଭିନ୍ନ ଦିଗକୁ ରେକର୍ଡ କର, ଯେପରି ଏଥିରେ ବର୍ଣ୍ଣନା କରାଯାଇଛି |
ବିଭାଗ ବ ly କଳ୍ପିକ ଭାବରେ, ଆପଣ ପ୍ରତ୍ୟେକ ପିଲାଙ୍କ ପାଇଁ କିଛି ପୃଷ୍ଠା ପ୍ରଦାନ କରୁଥିବା ଏକ ରେଜିଷ୍ଟର ମଧ୍ୟ ବ୍ୟବହାର କରିପାରିବେ |
ଏହି ରେକର୍ଡ ଏକ ପ୍ରସ୍ତୁତ ରେଫରେନ୍ସ କିମ୍ବା ଆପଣ ଏବଂ ଡାକ୍ତର / ସ୍ୱାସ୍ଥ୍ୟ ଭାବରେ କାର୍ଯ୍ୟ କରିବେ |
ଶ୍ରମିକ ନିମ୍ନଲିଖିତ ଦିଗଗୁଡ଼ିକ ବିଷୟରେ ଅନେକ ତଥ୍ୟ ମିଳିବ |
ମାତା ସେ କେନ୍ଦ୍ର ପରିଦର୍ଶନ ସମୟରେ ଆପଣ ତାଙ୍କ ସହିତ କଥା ହୋଇପାରନ୍ତି କିମ୍ବା ଆପଣଙ୍କୁ ଆବଶ୍ୟକ ହୋଇପାରେ |
ଘରେ ତାଙ୍କୁ ଦେଖା କର |
उसका वातावरण। इस उद्देश्य के लिए, यह उपयोगी होगा यदि आपके पास प्रत्येक के लिए एक कार्ड है
बच्चा जिसमें आप विभिन्न पहलुओं को रिकॉर्ड करते हैं, बच्चे के स्वास्थ्य पर ध्यान दिया जाता है, जैसा कि इसमें वर्णित है
अनुभाग। वैकल्पिक रूप से, आप प्रत्येक बच्चे के लिए कुछ पृष्ठ देने वाले रजिस्टर का भी उपयोग कर सकते हैं।
यह रिकॉर्ड एक तैयार संदर्भ या आप के साथ-साथ डॉक्टर / स्वास्थ्य के रूप में काम करेगा
कार्यकर्ता। निम्नलिखित पहलुओं के बारे में अधिक जानकारी से प्राप्त किया जाएगा
माता। आप केंद्र में उसकी यात्रा के दौरान उससे बात कर सकते हैं या आपको जरूरत पड़ सकती है
उसके घर पर जाएँ।
condition of the mother during pregnancy. It is important to establish a good
rapport with the child’s mother before you begin asking her about her pregnancy.
Ask her the following questions.
Did she have a full-term pregnancy?
Did she have any illness during her pregnancy, specifically Rubella (German
measles) or any other virus infection?
Did she have a fall or bleeding at any time during her pregnancy?
Did she take any drugs or medicines, or was she exposed to X-rays during her
pregnancy, especially during the first three months?
Did she take anti-tetanus injections?
ଗର୍ଭାବସ୍ଥାରେ ମାତାର ଅବସ୍ଥା | ଏକ ଭଲ ପ୍ରତିଷ୍ଠା କରିବା ଗୁରୁତ୍ୱପୂର୍ଣ୍ଣ |
ଆପଣ ତାଙ୍କ ଗର୍ଭଧାରଣ ବିଷୟରେ ପଚାରିବା ଆରମ୍ଭ କରିବା ପୂର୍ବରୁ ଶିଶୁର ମା ସହିତ ସମ୍ପର୍କ କରନ୍ତୁ |
ତାଙ୍କୁ ନିମ୍ନ ପ୍ରଶ୍ନ ପଚାର |
ତାଙ୍କର ପୂର୍ଣ୍ଣକାଳୀନ ଗର୍ଭଧାରଣ ଥିଲା କି?
ଗର୍ଭାବସ୍ଥାରେ ତାଙ୍କର କ illness ଣସି ରୋଗ ହୋଇଥିଲା କି, ବିଶେଷ ଭାବରେ ରୁବେଲା (ଜର୍ମାନ୍) |
ମିଳିମିଳା) କିମ୍ବା ଅନ୍ୟ କ virus ଣସି ଜୀବାଣୁ ସଂକ୍ରମଣ?
ଗର୍ଭଧାରଣ ସମୟରେ ସେ କ fall ଣସି ସମୟରେ ପତନ କିମ୍ବା ରକ୍ତସ୍ରାବ କରିଥିଲେ କି?
ସେ କ drugs ଣସି drugs ଷଧ କିମ୍ବା medicines ଷଧ ସେବନ କରିଥିଲେ ନା ତାଙ୍କ ସମୟରେ ଏକ୍ସ-ରେ ସଂସ୍ପର୍ଶରେ ଆସିଥିଲେ
ଗର୍ଭଧାରଣ, ବିଶେଷକରି ପ୍ରଥମ ତିନି ମାସ ମଧ୍ୟରେ?
ସେ ଆଣ୍ଟି-ଟିଟାନସ୍ ଇଞ୍ଜେକ୍ସନ ନେଇଥିଲେ କି?
गर्भावस्था के दौरान मां की स्थिति। एक अच्छा स्थापित करना महत्वपूर्ण है
इससे पहले कि आप उसकी गर्भावस्था के बारे में पूछना शुरू करें, बच्चे की माँ के साथ तालमेल बिठाएँ।
उससे निम्नलिखित प्रश्न पूछें।
क्या उसे पूर्ण अवधि का गर्भ था?
क्या उसे गर्भावस्था के दौरान कोई बीमारी थी, विशेष रूप से रूबेला (जर्मन)
खसरा) या कोई अन्य वायरस संक्रमण?
क्या गर्भावस्था के दौरान किसी भी समय उसे गिरने या रक्तस्राव हुआ था?
क्या उसने कोई ड्रग्स या दवाइयाँ लीं, या वह उसके दौरान एक्स-रे के संपर्क में थी
गर्भावस्था, विशेष रूप से पहले तीन महीनों के दौरान?
क्या उसने एंटी-टेटनस इंजेक्शन लिया था?
have read about care to be taken during delivery and care of the newborn in Unit 11,
Block 3 of this course. Ask the following questions to the mother regarding the birth
of the child.
Who conducted the delivery-a doctor/nurse/dai (trained/untrained)many other?
Was the birth process normal?
Was it full-term?
Did the baby have any problems during the process of delivery?
Did the child cry as soon as she was born?
What was the baby’s weight at birth?
Did the doctor or the dai tell her that the infant was normal?
births can affect the infant by depriving her of oxygen to the brain. Birth before term
or birth weight below normative range (i.e., below 2500 gms.) puts the infant in the
high risk category.
ୟୁନିଟ୍ 11 ରେ ନବଜାତ ଶିଶୁର ପ୍ରସବ ଏବଂ ଯତ୍ନ ନେବା ସମୟରେ ଯତ୍ନ ନେବାକୁ ପ read ିଛନ୍ତି,
ଏହି ପାଠ୍ୟକ୍ରମର 3 କୁ ଅବରୋଧ କରନ୍ତୁ | ଜନ୍ମ ବିଷୟରେ ମାତାଙ୍କୁ ନିମ୍ନଲିଖିତ ପ୍ରଶ୍ନ ପଚାର |
ଶିଶୁର
ସେ ପ୍ରସବକାଳୀନ ସ୍ୱାସ୍ଥ୍ୟ ପରିଦର୍ଶନ ପାଇଁ ଯାଇଥିଲେ କି?
କିଏ ପ୍ରସବ-ଡାକ୍ତର / ନର୍ସ / ଡାଏ (ତାଲିମପ୍ରାପ୍ତ / ତାଲିମପ୍ରାପ୍ତ) ପରିଚାଳନା କରିଥିଲେ?
ଜନ୍ମ ପ୍ରକ୍ରିୟା ସ୍ୱାଭାବିକ ଥିଲା କି?
ଏହା ପୂର୍ଣ୍ଣକାଳୀନ ଥିଲା କି?
ପ୍ରସବ ସମୟରେ ଶିଶୁର କ problems ଣସି ଅସୁବିଧା ହୋଇଥିଲା କି?
ନବଜାତ ଶିଶୁ କଷ୍ଟରେ ଥିଲେ କି?
କ res ଣସି ପୁନରୁଦ୍ଧାର ପଦକ୍ଷେପ ବ୍ୟବହୃତ ହୋଇଥିଲା କି?
ପିଲାଟି ଜନ୍ମ ହେବା ମାତ୍ରେ କାନ୍ଦିଲା କି?
ଜନ୍ମ ସମୟରେ ଶିଶୁର ଓଜନ କ’ଣ ଥିଲା?
ଡାକ୍ତର କିମ୍ବା ଡାଏ ତାଙ୍କୁ କହିଥିଲେ ଯେ ଶିଶୁଟି ସ୍ୱାଭାବିକ ଥିଲା?
ଏହି ସମସ୍ତ ପ୍ରଶ୍ନ ଗୁରୁତ୍ୱପୂର୍ଣ୍ଣ କାରଣ ବିତରଣ ସମୟରେ ବିଳମ୍ବ କିମ୍ବା ଜଟିଳ |
ଜନ୍ମ ଶିଶୁକୁ ମସ୍ତିଷ୍କକୁ ଅମ୍ଳଜାନରୁ ବଞ୍ଚିତ କରି ପ୍ରଭାବିତ କରିପାରିବ | ଅବଧି ପୂର୍ବରୁ ଜନ୍ମ |
କିମ୍ବା ଜନ୍ମ ଓଜନ ସାଧାରଣ ପରିସରଠାରୁ କମ୍ (ଯଥା, 2500 ଗ୍ରାମ ତଳେ) ଶିଶୁକୁ ରଖେ |
ଉଚ୍ଚ ବିପଦ ବର୍ଗ |
यूनिट 11 में नवजात की देखभाल और प्रसव के दौरान देखभाल के बारे में पढ़ा है,
इस कोर्स के ब्लॉक 3। जन्म के संबंध में माँ से निम्नलिखित प्रश्न पूछें
बच्चे का।
क्या वह प्रसवपूर्व स्वास्थ्य यात्राओं के लिए गई थीं?
किसने प्रसूति-एक डॉक्टर / नर्स / दाई (प्रशिक्षित / अप्रशिक्षित) का संचालन किया?
क्या जन्म प्रक्रिया सामान्य थी?
क्या यह पूर्ण-कालिक था?
क्या प्रसव की प्रक्रिया के दौरान शिशु को कोई समस्या थी?
क्या नवजात शिशु संकट में था?
क्या कोई पुनर्जीवन उपायों का इस्तेमाल किया गया था?
क्या बच्चा पैदा होते ही रोने लगा था?
जन्म के समय बच्चे का वजन कितना था?
क्या डॉक्टर या दाई ने उसे बताया कि शिशु सामान्य था?
ये सभी प्रश्न महत्वपूर्ण हैं क्योंकि प्रसव या जटिल के दौरान देरी
जन्म मस्तिष्क को ऑक्सीजन से वंचित करके शिशु को प्रभावित कर सकता है। कार्यकाल से पहले जन्म
या जन्म के बाद का वजन आदर्श सीमा (यानी 2500 ग्राम से नीचे) शिशु को अंदर डालता है
उच्च जोखिम श्रेणी।
the child’s health status. Taking the family history can help you to detect a health-
related problem in the child before it actually shows itself. This will enable you to
take preventive action and save precious time. Ask the following questions to know
the family history. How many brothers and sisters does the child have? Are any of
them sick? Have any died?
Does any family member have a chronic disease or illness?
A detailed family history may indicate the presence of genetic disorders that are
hereditary, such as haemophilia, or thalassefia. The family history may also show
some family members as having tuberculosis, malaria or amoebiasis. This indicates
that the environment the child lives in harbours such infections and the child is at
risk of acquiring them.
बच्चे की स्वास्थ्य स्थिति। स्वास्थ्य का पता लगाने के लिए परिवार के इतिहास को जानने में आपकी मदद कर सकते हैं-
इससे पहले कि यह वास्तव में खुद को दिखाता है बच्चे में संबंधित समस्या। यह आपको सक्षम करेगा
निवारक कार्रवाई करें और कीमती समय बचाएं। जानने के लिए निम्नलिखित प्रश्न पूछें
परिवार का इतिहास। बच्चे के कितने भाई-बहन हैं? किसी भी हो
उन्हें बीमार? कोई मर गया क्या?
क्या परिवार के किसी सदस्य को कोई पुरानी बीमारी या बीमारी है?
एक विस्तृत पारिवारिक इतिहास आनुवंशिक विकारों की उपस्थिति का संकेत दे सकता है जो हैं
वंशानुगत, जैसे कि हेमोफिलिया, या थैलासेफिया। परिवार का इतिहास भी दिखा सकता है
तपेदिक, मलेरिया या अमीबासिस के रूप में कुछ परिवार के सदस्य। यह इंगित करता है
यह कि बच्चा ऐसे संक्रमणों में रहता है और बच्चा जिस वातावरण में रहता है
उन्हें प्राप्त करने का जोखिम।
ଶିଶୁର ସ୍ୱାସ୍ଥ୍ୟ ସ୍ଥିତି ପାରିବାରିକ ଇତିହାସ ଗ୍ରହଣ କରିବା ଆପଣଙ୍କୁ ଏକ ସ୍ୱାସ୍ଥ୍ୟ ଚିହ୍ନଟ କରିବାରେ ସାହାଯ୍ୟ କରିପାରିବ-
ପିଲାଟି ପ୍ରକୃତରେ ନିଜକୁ ଦେଖାଇବା ପୂର୍ବରୁ ସମ୍ବନ୍ଧୀୟ ସମସ୍ୟା | ଏହା ଆପଣଙ୍କୁ ସକ୍ଷମ କରିବ |
ପ୍ରତିଷେଧକ ପଦକ୍ଷେପ ନିଅ ଏବଂ ମୂଲ୍ୟବାନ ସମୟ ସଞ୍ଚୟ କର | ଜାଣିବା ପାଇଁ ନିମ୍ନଲିଖିତ ପ୍ରଶ୍ନ ପଚାରନ୍ତୁ |
ପରିବାର ଇତିହାସ ପିଲାଟିର କେତେ ଭାଇ ଓ ଭଉଣୀ ଅଛନ୍ତି? ମଧ୍ୟରୁ କ are ଣସିଟି ଅଛି |
ସେମାନେ ଅସୁସ୍ଥ କି? କେହି ମରିଛନ୍ତି କି?
କ family ଣସି ପରିବାରର ସଦସ୍ୟଙ୍କର କ୍ରନିକ ରୋଗ ବା ଅସୁସ୍ଥତା ଅଛି କି?
ଏକ ବିସ୍ତୃତ ପରିବାର ଇତିହାସ ଜେନେଟିକ୍ ବ୍ୟାଧିଗୁଡିକର ଉପସ୍ଥିତି ସୂଚାଇପାରେ |
ବଂଶାନୁକ୍ରମିକ, ଯେପରିକି ହେମୋଫିଲିଆ, କିମ୍ବା ଥାଲାସେଫିଆ | ପାରିବାରିକ ଇତିହାସ ମଧ୍ୟ ଦେଖାଇପାରେ |
କେତେକ ପରିବାର ସଦସ୍ୟ ଯକ୍ଷ୍ମା, ମ୍ୟାଲେରିଆ କିମ୍ବା ଆମୋବିଆସିସ୍ ରୋଗରେ ଆକ୍ରାନ୍ତ | ଏହା ସୂଚିତ କରେ |
ଶିଶୁଟି ଏପରି ସଂକ୍ରମଣରେ ବାସ କରୁଥିବା ପରିବେଶ ଏବଂ ଶିଶୁଟି ଅଛି |
ସେଗୁଡିକ ହାସଲ କରିବାର ବିପଦ |
Obtain as complete an account of these as possible,
What were the illnesses?
What was the course of the disease in each case?
How was each illness treated?
Did the child recover completely?
How long did the illness last?
How long did convalescence take?
Are there any after-effects?
ଯଥାସମ୍ଭବ ଏଗୁଡିକର ଏକ ଆକାଉଣ୍ଟ୍ ପ୍ରାପ୍ତ କରନ୍ତୁ,
ରୋଗଗୁଡିକ କ’ଣ ଥିଲା?
ପ୍ରତ୍ୟେକ କ୍ଷେତ୍ରରେ ରୋଗର ଗତି କ’ଣ ଥିଲା?
ପ୍ରତ୍ୟେକ ରୋଗ କିପରି ଚିକିତ୍ସା କରାଗଲା?
ପିଲାଟି ସମ୍ପୂର୍ଣ୍ଣ ସୁସ୍ଥ ହୋଇଗଲା କି?
ରୋଗ କେତେ ଦିନ ପର୍ଯ୍ୟନ୍ତ ରହିଲା?
ସୁସ୍ଥତା କେତେ ସମୟ ନେଇଥିଲା?
କିଛି ପରବର୍ତ୍ତୀ ପ୍ରଭାବ ଅଛି କି?
जितना संभव हो, इनमें से एक खाते को पूरा करें।
क्या बीमारियाँ थीं?
प्रत्येक मामले में बीमारी का कोर्स क्या था?
प्रत्येक बीमारी का इलाज कैसे किया गया?
क्या बच्चा पूरी तरह से ठीक हो गया?
बीमारी कब तक चली?
दीक्षांत समारोह में कितना समय लगा?
क्या कोई आफ्टर-इफेक्ट्स हैं?
an illness may be very obvious and the mother hill most likely tell you about it,
when you ask her. But sometimes, the illness may not be evident to the mother or
she may not think much of the symptoms and, therefore, not mention them. In this
case, you must ask specific probing questions. For example, the child may have night
blindness but the mother may not have noticed it or, does not give it much
bicomimportance. Therefore, ask questions like: “
“Does he or she bump into things at night?”
In another instance, the child may not have fever when you see her, but on
questioning you may find that mother reports intermittent fever, with shivering
occurring at regular intervals. It could be malaria.
Ask the parent questions that will help you to know whether or not the child’s level
of cognitive development is in keeping with the norms of her age. Similarly, try to
find out about the child’s social and emotional adjustinent. You have read about
milestones of development in the various Blocks of DECE-1. Find out when the child
learnt to recognize the mother/parent and others, to identify and name objects.
Discover if the child is active and responsive, and is being socialized to interact
cooperatively with her/his family.
एक बीमारी बहुत स्पष्ट हो सकती है और माता पहाड़ी सबसे अधिक आपको इसके बारे में बताती है,
जब आप उससे पूछें। लेकिन कभी-कभी, बीमारी माँ को स्पष्ट नहीं हो सकती है या
वह लक्षणों के बारे में ज्यादा नहीं सोच सकती है और इसलिए, उनका उल्लेख नहीं करती है। इसमें
मामला, आपको विशिष्ट जांच प्रश्न पूछना चाहिए। उदाहरण के लिए, बच्चे को रात हो सकती है
अंधापन लेकिन माँ ने इस पर ध्यान नहीं दिया होगा या इसे ज्यादा नहीं दिया है
bicomimportance। इसलिए, जैसे सवाल पूछें: ”
क्या बच्चे को अंधेरे में घूमने में कोई कठिनाई होती है? ‘
“क्या वह रात में चीजों से टकराता है?”
एक अन्य उदाहरण में, जब आप उसे देखते हैं तो बच्चे को बुखार नहीं हो सकता है
सवाल यह है कि आपको लग सकता है कि माँ कंपकंपी के साथ रुक-रुक कर बुखार आने की रिपोर्ट करती है
नियमित अंतराल पर होने वाली। यह मलेरिया हो सकता है।
अभिभावक प्रश्न पूछें जो आपको यह जानने में मदद करेगा कि बच्चे का स्तर है या नहीं
संज्ञानात्मक विकास उसकी उम्र के मानदंडों को ध्यान में रखते हुए है। इसी तरह, प्रयास करें
बच्चे के सामाजिक और भावनात्मक समायोजन के बारे में पता करें। आप के बारे में पढ़ा है
DECE-1 के विभिन्न ब्लॉकों में विकास के मील के पत्थर। बच्चे का पता लगाएं
माँ / माता-पिता और अन्य लोगों को पहचानना, वस्तुओं को पहचानना और नाम देना सीखा।
पता लगाएँ कि क्या बच्चा सक्रिय और उत्तरदायी है, और बातचीत करने के लिए समाजीकरण किया जा रहा है
उसके / उसके परिवार के साथ सहकारी रूप से।
ଏକ ରୋଗ ଅତ୍ୟନ୍ତ ସ୍ପଷ୍ଟ ହୋଇପାରେ ଏବଂ ମାତା ପାହାଡ ସମ୍ଭବତ you ଆପଣଙ୍କୁ ଏହା ବିଷୟରେ କହିବ,
ଯେତେବେଳେ ତୁମେ ତାଙ୍କୁ ପଚାରିବ କିନ୍ତୁ ବେଳେବେଳେ, ଏହି ରୋଗ ମା ପାଇଁ ସ୍ପଷ୍ଟ ହୋଇନପାରେ କିମ୍ବା |
ସେ ହୁଏତ ଅନେକ ଲକ୍ଷଣ ବିଷୟରେ ଚିନ୍ତା କରିପାରନ୍ତି ନାହିଁ, ତେଣୁ, ସେଗୁଡିକ ବିଷୟରେ ଉଲ୍ଲେଖ କରନ୍ତୁ ନାହିଁ | ଏଥିରେ
କେସ୍, ଆପଣ ନିଶ୍ଚିତ ଭାବରେ ନିର୍ଦ୍ଦିଷ୍ଟ ଅନୁସନ୍ଧାନ ପ୍ରଶ୍ନ ପଚାରିବେ | ଉଦାହରଣ ସ୍ୱରୂପ, ପିଲାଟି ରାତି ହୋଇପାରେ |
ଅନ୍ଧତା କିନ୍ତୁ ମା ହୁଏତ ଏହା ଜାଣି ନଥିବେ କିମ୍ବା, ଏହାକୁ ଅଧିକ ଦିଅନ୍ତି ନାହିଁ |
bicomimportance ତେଣୁ, ଏହିପରି ପ୍ରଶ୍ନ ପଚାର: ”
ଅନ୍ଧାରରେ ବୁଲିବାରେ ପିଲାଟିର କ difficulty ଣସି ଅସୁବିଧା ଅଛି କି? ‘,
ସେ ରାତିରେ ଜିନିଷରେ ump ୁଣ୍ଟି ପଡ଼ନ୍ତି କି?
ଅନ୍ୟ ଏକ ପରିସ୍ଥିତିରେ, ଯେତେବେଳେ ଆପଣ ତାଙ୍କୁ ଦେଖିବେ ପିଲାଟି ଜ୍ୱର ହୋଇନପାରେ, କିନ୍ତୁ
ପ୍ରଶ୍ନ କରିବା ଦ୍ you ାରା ଆପଣ ଜାଣିପାରିବେ ଯେ ମାତା ଥରି ଥରି ମଧ୍ୟବର୍ତ୍ତୀ ଜ୍ୱର ରିପୋର୍ଟ କରନ୍ତି |
ନିୟମିତ ବ୍ୟବଧାନରେ ଘଟୁଛି | ଏହା ମ୍ୟାଲେରିଆ ହୋଇପାରେ |
ପିତାମାତାଙ୍କ ପ୍ରଶ୍ନ ପଚାରନ୍ତୁ ଯାହା ଆପଣଙ୍କୁ ଶିଶୁର ସ୍ତର ଅଛି କି ନାହିଁ ଜାଣିବାରେ ସାହାଯ୍ୟ କରିବ |
ଜ୍ ogn ାନକ development ଶଳ ବିକାଶ ତାଙ୍କ ବୟସର ମାନଦଣ୍ଡ ସହିତ ଅଟେ | ସେହିଭଳି, ଚେଷ୍ଟା କରନ୍ତୁ |
ଶିଶୁର ସାମାଜିକ ଏବଂ ଭାବପ୍ରବଣତା ବିଷୟରେ ଜାଣନ୍ତୁ | ଆପଣ ପ read ିଛନ୍ତି
DECE-1 ର ବିଭିନ୍ନ ବ୍ଲକରେ ବିକାଶର ମାଇଲଖୁଣ୍ଟ | ପିଲାଟି କେବେ ଖୋଜ |
ମାତା / ପିତାମାତା ଏବଂ ଅନ୍ୟମାନଙ୍କୁ ଚିହ୍ନିବା, ବସ୍ତୁଗୁଡ଼ିକୁ ଚିହ୍ନିବା ଏବଂ ନାମକରଣ କରିବା ଶିଖିଲେ |
ପିଲାଟି ସକ୍ରିୟ ଏବଂ ପ୍ରତିକ୍ରିୟାଶୀଳ କି ନାହିଁ, ଏବଂ ପାରସ୍ପରିକ ଭାବରେ ସାମାଜିକ ହେବା ପାଇଁ ଆବିଷ୍କାର କର |
ତାଙ୍କ ପରିବାର ସହିତ ସହଯୋଗରେ |
out in considerable detail the child’s nutrition history.
Is or was the child breast fed?
When was breast feeding stopped?
of dilution, and methods of sterilization for feeder.
If the child is already four months of age, ask
What foods does the child eat?
If the child is older, ask
When was this started?
In addition, explore par`ents’ and/or child’s food preferences, special likes/dislikes,
norms is one way of knowing whether the child is growing ‘normally’ or not.
Milestones or norms, as you know, are indicators of average growth.
6 weeks – smiles; recognizes mother
12-16 weeks – rolls over from back to front, or vice versa
7-8 months – sits upright without help
13-15 months – walks
13-15months – talks in single words
will have to ask questions like: “When did the child begin to recognize you?”, “When
did she begin to hold her head without support? Parent may not remember some
specific development. This does not matter, so long as you get a general picture. You
can also get a picture by asking if this child is growing like other siblings. Besides
asking these questions to the parent, be observant of the child’s behavior. This can
tell you a lot about the child’s level of development. A child’s growth pattern should,
by and large, follow the milestones or norms of development: Of course, these
milestones are not rigid. A child may lag behind or move ahead a month or two as
compared to these norms. Slight variations are not a cause of worry. However, if a
child’s development in any or most areas lags behind considerably Childhood as
compared to these norms, then it is a cause for concern. The reason for this could be
illness or nutritional deficiency or retardation or some emotional problem.
ପୁଷ୍ଟିକର ଇତିହାସ: —
ପୁଷ୍ଟିକର ସ୍ୱାସ୍ଥ୍ୟ ସେବାର ଏକ ଅବିଚ୍ଛେଦ୍ୟ ଅଙ୍ଗ ହୋଇଥିବାରୁ ଆପଣଙ୍କୁ ଖୋଜିବାକୁ ପଡ଼ିବ |
ଶିଶୁର ପୁଷ୍ଟିକର ଇତିହାସ ବିଷୟରେ ବିସ୍ତୃତ ଭାବରେ |
ଶିଶୁକୁ ସ୍ତନ୍ୟପାନ କରାଗଲା କି?
ସ୍ତନ୍ୟପାନ କେବେ ବନ୍ଦ ହେଲା?
ମିଶ୍ରଣ ଏବଂ ଫିଡର୍ ପାଇଁ ନିରାକରଣର ପଦ୍ଧତି |
ଯଦି ପିଲାଟି ଚାରିମାସ ବୟସ ହୋଇସାରିଛି, ପଚାରନ୍ତୁ |
ପିଲା କେଉଁ ଖାଦ୍ୟ ଖାଏ?
ଯଦି ପିଲାଟି ବଡ, ପଚାରନ୍ତୁ |
ସେ ସାଧାରଣ ବୟସ୍କ ଖାଦ୍ୟ ଖାଏ କି?
ଏହା କେବେ ଆରମ୍ଭ ହେଲା?
ଶିଶୁର ଭୋକ ସ୍ୱାଭାବିକ କି?
ଏହା ସହିତ, ପ୍ୟାରେଣ୍ଟସ୍ ଏବଂ / କିମ୍ବା ଶିଶୁର ଖାଦ୍ୟ ପସନ୍ଦ, ବିଶେଷ ପସନ୍ଦ / ନାପସନ୍ଦ,
ଅଭିବୃଦ୍ଧି ଇତିହାସ: ବିକାଶର ମାଇଲଖୁଣ୍ଟ ସହିତ ଶିଶୁର ବୃଦ୍ଧିକୁ ତୁଳନା କରିବା କିମ୍ବା
ପିଲାଟି ‘ସାଧାରଣ’ ବ growing ୁଛି କି ନାହିଁ ଜାଣିବାର ଏକ ଉପାୟ |
ମାଇଲଷ୍ଟୋନ ବା ଆଦର୍ଶ, ଯେପରି ଆପଣ ଜାଣନ୍ତି, ହାରାହାରି ଅଭିବୃଦ୍ଧିର ସୂଚକ |
6 ସପ୍ତାହ – ହସ; ମାତାଙ୍କୁ ଚିହ୍ନିଥାଏ |
12-16 ସପ୍ତାହ – ପଛରୁ ଆଗକୁ ଗଡ଼େ, କିମ୍ବା ବିପରୀତରେ |
7-8 ମାସ – ବିନା ସାହାଯ୍ୟରେ ସିଧା ବସିଥାଏ |
13-15 ମାସ – ଚାଲନ୍ତି |
13-15 ମାସ – ଏକକ ଶବ୍ଦରେ କଥାବାର୍ତ୍ତା |
ଶିଶୁର ବିକାଶ ଏହି ନିୟମ ମାନିଛି କି ନାହିଁ ମାତା / ପିତାମାତାଙ୍କୁ ପଚାରନ୍ତୁ | ତୁମେ
ଏହିପରି ପ୍ରଶ୍ନ ପଚାରିବାକୁ ପଡ଼ିବ: “ପିଲାଟି ତୁମକୁ ଚିହ୍ନିବା ଆରମ୍ଭ କଲା?”, “କେତେବେଳେ
ସେ ସମର୍ଥନ ବିନା ମୁଣ୍ଡ ଧରିବାକୁ ଲାଗିଲେ କି? ପିତାମାତା ହୁଏତ କିଛି ମନେ ରଖିପାରନ୍ତି ନାହିଁ |
ନିର୍ଦ୍ଦିଷ୍ଟ ବିକାଶ ଯେପର୍ଯ୍ୟନ୍ତ ଆପଣ ଏକ ସାଧାରଣ ଚିତ୍ର ପାଇବେ, ସେଥିରେ କିଛି ଫରକ ପଡ଼ିବ ନାହିଁ | ତୁମେ
ଏହି ପିଲାଟି ଅନ୍ୟ ଭାଇଭଉଣୀଙ୍କ ପରି ବ growing ୁଛି କି ନାହିଁ ପଚାରି ଏକ ଚିତ୍ର ମଧ୍ୟ ପାଇପାରିବ | ଏହା ବ୍ୟତୀତ |
ପିତାମାତାଙ୍କୁ ଏହି ପ୍ରଶ୍ନ ପଚାରିବା, ଶିଶୁର ଆଚରଣ ଉପରେ ନଜର ରଖ | ଏହା ହୋଇପାରେ |
ଶିଶୁର ବିକାଶ ସ୍ତର ବିଷୟରେ ଆପଣଙ୍କୁ ବହୁତ କିଛି କହିବ | ଏକ ଶିଶୁର ଅଭିବୃଦ୍ଧି pattern ାଞ୍ଚା,
ଏବଂ ବୃହତ ଭାବରେ, ମାଇଲଖୁଣ୍ଟ କିମ୍ବା ବିକାଶର ଆଦର୍ଶ ଅନୁସରଣ କରନ୍ତୁ: ଅବଶ୍ୟ, ଏଗୁଡ଼ିକ |
ମାଇଲଖୁଣ୍ଟ କଠିନ ନୁହେଁ | ଏକ ଶିଶୁ ଏକ ମାସ କିମ୍ବା ଦୁଇ ମାସ ପରି ଆଗକୁ ଯାଇପାରେ |
ଏହି ଆଦର୍ଶଗୁଡ଼ିକ ତୁଳନାରେ ସାମାନ୍ୟ ପରିବର୍ତ୍ତନ ଚିନ୍ତାର କାରଣ ନୁହେଁ | ଯଦିଓ, ଯଦି a
ଯେକ any ଣସି କିମ୍ବା ଅଧିକାଂଶ କ୍ଷେତ୍ରରେ ଶିଶୁର ବିକାଶ ବାଲ୍ୟକାଳ ପରି ବହୁ ପଛରେ ରହିଥାଏ |
ଏହି ଆଦର୍ଶଗୁଡ଼ିକ ତୁଳନାରେ, ତେବେ ଏହା ଚିନ୍ତାର କାରଣ | ଏହାର କାରଣ ହୋଇପାରେ |
ଅସୁସ୍ଥତା କିମ୍ବା ପୁଷ୍ଟିକର ଅଭାବ କିମ୍ବା ଅବସାଦ କିମ୍ବା କିଛି ଭାବପ୍ରବଣ ସମସ୍ୟା |
पोषण इतिहास: —
पोषण स्वास्थ्य देखभाल का एक अभिन्न अंग होने के नाते, आपको खोजने की आवश्यकता है
बच्चे के पोषण के इतिहास में काफी विस्तार से।
क्या बच्चे को स्तनपान कराया गया था?
स्तनपान कब बंद कर दिया गया था?
पतला करने के लिए, और फीडर के लिए नसबंदी के तरीके।
यदि बच्चा पहले से ही चार महीने का है, तो पूछें
बच्चा क्या खाद्य पदार्थ खाता है?
यदि बच्चा बड़ा है, तो पूछें
वह एक सामान्य वयस्क आहार खाती है या नहीं?
यह कब शुरू किया गया था?
क्या बच्चे का एपेटाइट सामान्य है?
इसके अलावा, माता-पिता का पता लगाएं और / या बच्चे की खाद्य प्राथमिकताएं, विशेष पसंद / नापसंद,
विकास का इतिहास: विकास के मील के पत्थर के साथ बच्चे की वृद्धि की तुलना करना या
मानदंड यह जानने का एक तरीका है कि क्या बच्चा सामान्य रूप से बढ़ रहा है या नहीं।
मील के पत्थर या मानदंड, जैसा कि आप जानते हैं, औसत वृद्धि के संकेतक हैं।
6 सप्ताह – मुस्कुराहट; माँ को पहचानता है
12-16 सप्ताह – पीछे से आगे की तरफ, या इसके विपरीत रोल
7-8 महीने – बिना मदद के सीधा बैठता है
13-15 महीने – चलता है
13-15 महीने – एकल शब्दों में बात करता है
माँ / माता-पिता से पूछें कि क्या बच्चे के विकास ने इन मानदंडों का पालन किया है। आप
जैसे प्रश्न पूछना होगा: “बच्चे ने आपको कब पहचाना?”, “कब
क्या उसने बिना सहारे के अपना सिर पकड़ना शुरू कर दिया? माता-पिता को शायद कुछ याद न हो
विशिष्ट विकास। इससे कोई फर्क नहीं पड़ता, इसलिए जब तक आपको एक सामान्य तस्वीर मिलती है। आप
यह भी पूछ सकते हैं कि क्या यह बच्चा अन्य भाई-बहनों की तरह बढ़ रहा है। के अतिरिक्त
माता-पिता से ये सवाल पूछते हुए, बच्चे के व्यवहार के प्रति चौकस रहें। यह हो सकता है
आपको बच्चे के विकास के स्तर के बारे में बहुत कुछ बताते हैं। एक बच्चे का विकास पैटर्न,
द्वारा और बड़े, मील के पत्थर या विकास के मानदंडों का पालन करें: बेशक, ये
मील के पत्थर कठोर नहीं हैं। एक बच्चा एक या दो महीने पीछे रह सकता है या आगे बढ़ सकता है
इन मानदंडों की तुलना में। थोड़ा बदलाव चिंता का कारण नहीं है। हालांकि, अगर ए
किसी भी या अधिकांश क्षेत्रों में बच्चे का विकास काफी बचपन से पिछड़ जाता है
इन मानदंडों की तुलना में, तो यह चिंता का कारण है। इसका कारण हो सकता है
बीमारी या पोषण की कमी या मंदता या कुछ भावनात्मक समस्या।
immunized. If yes, what injections have been given, and when. Also find out
whether oral anti-polio doses have been given. You will read about the schedule of
immunization a little later in the unit.
ପ୍ରତିରୋପଣ ଯଦି ହଁ, କେଉଁ ଇଞ୍ଜେକ୍ସନ ଦିଆଯାଇଛି, ଏବଂ କେବେ | ଏହା ମଧ୍ୟ ଖୋଜ |
ମ oral ଖିକ ଆଣ୍ଟି ପୋଲିଓ ମାତ୍ରା ଦିଆଯାଇଛି କି ନାହିଁ | ଆପଣ କାର୍ଯ୍ୟସୂଚୀ ବିଷୟରେ ପ read ିବେ |
ୟୁନିଟରେ ଟିକିଏ ପରେ ପ୍ରତିରୋପଣ |
प्रतिरक्षित। यदि हाँ, तो कौन सा इंजेक्शन दिया गया है, और कब। यह भी पता करें
क्या मौखिक पोलियो रोधी खुराक दी गई है। के शेड्यूल के बारे में आप पढ़ेंगे
यूनिट में थोड़ी देर बाद टीकाकरण।
type of social and emotional environment the child lives in.
Whom does the child play with?
Is the child allowed to play in any part of the house?
Do the parents talk to the child and keep time for playing or answering questions?
Does the child have a chance to play outdoors, especially in sunlight?
Is it a safe environment?
ପିଲାଟି ରହୁଥିବା ସାମାଜିକ ଏବଂ ଭାବପ୍ରବଣ ପରିବେଶର ପ୍ରକାର |
ପିଲାଟି କାହା ସହିତ ଖେଳେ?
ପିଲାଟିର ଘରର କ part ଣସି ଅଂଶରେ ଖେଳିବାକୁ ଅନୁମତି ଦିଆଯାଇଛି କି?
ପିତାମାତା ପିଲାଙ୍କ ସହ କଥାବାର୍ତ୍ତା କରନ୍ତି ଏବଂ ପ୍ରଶ୍ନ ଖେଳିବା କିମ୍ବା ଉତ୍ତର ଦେବା ପାଇଁ ସମୟ ରଖନ୍ତି କି?
ବିଶେଷ କରି ସୂର୍ଯ୍ୟ କିରଣରେ ପିଲାଟି ବାହାରେ ଖେଳିବାର ସୁଯୋଗ ପାଇଥାଏ କି?
ଏହା ଏକ ସୁରକ୍ଷିତ ପରିବେଶ କି?
सामाजिक और पर्यावरणीय इतिहास: निम्नलिखित सवालों के बारे में जानने के लिए कहें
बच्चे में सामाजिक और भावनात्मक वातावरण का प्रकार।
बच्चा किसके साथ खेलता है?
क्या बच्चे को घर के किसी भी हिस्से में खेलने की अनुमति है?
क्या माता-पिता बच्चे से बात करते हैं और खेलने या सवालों के जवाब देने के लिए समय रखते हैं?
क्या बच्चे को बाहर का खेल खेलने का मौका मिलता है, खासकर धूप में?
क्या यह सुरक्षित वातावरण है?
prevalent among young children (0-6 years) but is also observed as starvation in
adolescents and adults, mostly lactating women, especially during periods of famine
or other emergencies. PEM has serious consequences for the health of individuals,
particularly, children and can even result in death.
छोटे बच्चों (0-6 वर्ष) के बीच प्रचलित है, लेकिन भुखमरी के रूप में भी मनाया जाता है
किशोरों और वयस्कों, ज्यादातर स्तनपान कराने वाली महिलाओं, विशेष रूप से अकाल की अवधि के दौरान
या अन्य आपात स्थिति। पीईएम के व्यक्तियों के स्वास्थ्य के लिए गंभीर परिणाम हैं,
विशेष रूप से, बच्चे और यहां तक कि मृत्यु भी हो सकती है।
ଛୋଟ ପିଲାମାନଙ୍କ ମଧ୍ୟରେ ପ୍ରଚଳିତ (0-6 ବର୍ଷ) କିନ୍ତୁ ଅନାହାରରେ ମଧ୍ୟ ଦେଖାଯାଏ |
ବିଶେଷକରି ଦୁର୍ଭିକ୍ଷ ସମୟରେ କିଶୋର ଏବଂ ବୟସ୍କମାନେ, ସ୍ତନ୍ୟପାନ କରାଉଥିବା ମହିଳା |
କିମ୍ବା ଅନ୍ୟାନ୍ୟ ଜରୁରୀକାଳୀନ ପରିସ୍ଥିତି | ବ୍ୟକ୍ତିବିଶେଷଙ୍କ ସ୍ୱାସ୍ଥ୍ୟ ପାଇଁ PEM ର ଗମ୍ଭୀର ପରିଣାମ ଅଛି,
ବିଶେଷକରି ପିଲାମାନେ ଏବଂ ଏପରିକି ମୃତ୍ୟୁ ମଧ୍ୟ ହୋଇପାରେ |
two forms:
a) Marasmus
b) Kwashiorkor
However, there are also children who show some of the characteristic signs of both
marasmus and kwashiorkor. Such children are said to suffer from Marasmic
Kwashiorkor, Then there are children whose heights and weights are considerably
below that of healthy children of the same age. These children may not show any
typical clinical signs of either kwashiorkor or marasmus, and as such they are placed
in the category of subclinical forms of PEM which forms a large proportion of the
disease in the community,
दो रूप:
a) Marasmus
b) क्वाशिओकोर
हालांकि, ऐसे बच्चे भी हैं जो दोनों के कुछ विशिष्ट लक्षण दिखाते हैं
marasmus और kwashiorkor। कहा जाता है कि इस तरह के बच्चों को मरासेमिक से पीड़ित होता है
Kwashiorkor, फिर ऐसे बच्चे हैं जिनकी हाइट और वज़न काफी कम है
उसी उम्र के स्वस्थ बच्चों के नीचे। हो सकता है कि ये बच्चे किसी को न दिखाए
kwashiorkor या marasmus के विशिष्ट नैदानिक संकेत, और जैसे उन्हें रखा गया है
PEM के उप-वर्गीय रूपों की श्रेणी में जो का एक बड़ा अनुपात बनाता है
समुदाय में बीमारी,
ଦୁଇଟି ଫର୍ମ:
କ) ମାରାସ୍ମସ୍ |
ଖ) କ୍ୱାସିୟର୍କର୍ |
ତଥାପି, ଏପରି କିଛି ପିଲା ମଧ୍ୟ ଅଛନ୍ତି, ଯେଉଁମାନେ ଉଭୟର କିଛି ଚରିତ୍ରଗତ ଲକ୍ଷଣ ଦେଖାନ୍ତି |
ମାରାସ୍ମସ୍ ଏବଂ କ୍ୱାସିୟର୍କର୍ ଏହିପରି ପିଲାମାନେ ମାର୍ସମିକ୍ ରୋଗରେ ପୀଡିତ ବୋଲି କୁହାଯାଏ
Kwashiorkor, ତା’ପରେ ଏପରି କିଛି ପିଲା ଅଛନ୍ତି ଯାହାର ଉଚ୍ଚତା ଏବଂ ଓଜନ ଯଥେଷ୍ଟ |
ସମାନ ବୟସର ସୁସ୍ଥ ପିଲାମାନଙ୍କ ତଳେ | ଏହି ପିଲାମାନେ ହୁଏତ କିଛି ଦେଖାଇ ପାରନ୍ତି ନାହିଁ |
kwashiorkor କିମ୍ବା marasmus ର ସାଧାରଣ କ୍ଲିନିକାଲ୍ ଚିହ୍ନ, ଏବଂ ସେଗୁଡିକ ସେଗୁଡିକ ରଖାଯାଇଥାଏ |
PEM ର ସବ୍କ୍ଲିନିକାଲ୍ ଫର୍ମ ବର୍ଗରେ ଯାହା ଏକ ବୃହତ ଅନୁପାତ ଗଠନ କରେ |
ସମ୍ପ୍ରଦାୟରେ ରୋଗ,

Subclinical forms of a disease, refer to the condition where external medical
examination may not show any signs of the disease. However, when we examine in
detail – by body measurements like weight or examination of blood – we can detect
changes. In the case of PEM, we can see a large number of subclinical forms.
children out of a hundred, in the age group of 1-5 years, exhibit these clinical forms
of PEM. However, many more subclinical cases of PEM – which cannot be easily
detected by simple clinical examination, are widely prevalent in the community. For
each case of kwashiorkor or marasmus, there may usually be 10 to 15 subclinical
cases of PEM. For prevention of PEM, we have to take steps by identifying such
cases so that prompt treatment or rehabilitation (helping child to recover his normal
health)-can be provided.
परीक्षा में बीमारी के कोई लक्षण नहीं दिख सकते हैं। हालाँकि, जब हम जांच करते हैं
विस्तार – शरीर के माप जैसे वजन या रक्त की जांच से – हम पता लगा सकते हैं
परिवर्तन। पीईएम के मामले में, हम बड़ी संख्या में उप-विषयक रूप देख सकते हैं।
Kwashiorkor और marasmus केवल एक हिमशैल की नोक हैं। हमारे देश में केवल 2-3
1-5 वर्ष के आयु समूह में सौ में से बच्चे इन नैदानिक रूपों का प्रदर्शन करते हैं
पेम की। हालाँकि, PEM के कई और अधिक उप-मामले – जो आसानी से नहीं हो सकते
साधारण नैदानिक परीक्षा से पता चला, समुदाय में व्यापक रूप से प्रचलित हैं। के लिये
kwashiorkor या marasmus के प्रत्येक मामले में, आमतौर पर 10 से 15 उपवर्ग हो सकते हैं
पीईएम के मामले। पीईएम की रोकथाम के लिए हमें इस तरह की पहचान करके कदम उठाने होंगे
ऐसे मामले जो शीघ्र उपचार या पुनर्वास करते हैं (बच्चे को उसकी सामान्य स्थिति को ठीक करने में मदद करते हैं
स्वास्थ्य) -न प्रदान किया जाएगा।
ପରୀକ୍ଷା ଦ୍ the ାରା ରୋଗର କ signs ଣସି ଲକ୍ଷଣ ଦେଖାଯାଇନପାରେ | ତଥାପି, ଯେତେବେଳେ ଆମେ ପରୀକ୍ଷା କରିବା |
ସବିଶେଷ – ଶରୀରର ମାପ ଦ୍ weight ାରା ଓଜନ କିମ୍ବା ରକ୍ତ ପରୀକ୍ଷା – ଆମେ ଚିହ୍ନଟ କରିପାରିବା |
ପରିବର୍ତ୍ତନ PEM କ୍ଷେତ୍ରରେ, ଆମେ ବହୁ ସଂଖ୍ୟକ ସବ୍କ୍ଲିନିକାଲ୍ ଫର୍ମ ଦେଖିପାରିବା |
କ୍ୱାସିୟର୍କର୍ ଏବଂ ମାରାସ୍ମସ୍ କେବଳ ଏକ ବରଫର ଏକ ଅଂଶ | ଆମ ଦେଶରେ କେବଳ 2-3
ଶହେରୁ children ର୍ଦ୍ଧ୍ୱ ପିଲାମାନେ, 1-5 ବର୍ଷ ବୟସ ବର୍ଗରେ, ଏହି କ୍ଲିନିକାଲ୍ ଫର୍ମଗୁଡିକ ପ୍ରଦର୍ଶନ କରନ୍ତି |
PEM ର ତଥାପି, PEM ର ଆହୁରି ଅନେକ ସବ୍କ୍ଲିନିକାଲ୍ କେସ୍ – ଯାହା ସହଜରେ ହୋଇପାରିବ ନାହିଁ |
ସରଳ କ୍ଲିନିକାଲ୍ ପରୀକ୍ଷଣ ଦ୍ୱାରା ଚିହ୍ନଟ, ସମ୍ପ୍ରଦାୟରେ ବହୁଳ ଭାବରେ ପ୍ରଚଳିତ | ପାଇଁ
kwashiorkor କିମ୍ବା marasmus ର ପ୍ରତ୍ୟେକ କ୍ଷେତ୍ରରେ, ସାଧାରଣତ 10 10 ରୁ 15 ସବ୍କ୍ଲିନିକାଲ୍ ହୋଇପାରେ |
PEM ର ମାମଲା | PEM ରୋକିବା ପାଇଁ, ଆମକୁ ଚିହ୍ନଟ କରି ପଦକ୍ଷେପ ନେବାକୁ ପଡିବ |
ମାମଲା ଯାହା ଦ୍ prompt ାରା ତୁରନ୍ତ ଚିକିତ୍ସା କିମ୍ବା ପୁନର୍ବାସ (ଶିଶୁକୁ ତାଙ୍କର ସ୍ୱାଭାବିକ ପୁନରୁଦ୍ଧାରରେ ସାହାଯ୍ୟ କରେ) |
ସ୍ୱାସ୍ଥ୍ୟ) – ଯୋଗାଇ ଦିଆଯାଇପାରେ |
sign. So then, how are these forms different from each other? The description below
presents a clear picture of the different forms of PEM and lists signs and symptoms
specific to each form, which will help us identify individuals suffering from different
संकेत। तो फिर, ये रूप एक-दूसरे से कैसे भिन्न हैं? नीचे विवरण
पीईएम के विभिन्न रूपों की एक स्पष्ट तस्वीर प्रस्तुत करता है और संकेतों और लक्षणों को सूचीबद्ध करता है
प्रत्येक रूप से विशिष्ट, जो हमें अलग-अलग पीड़ित व्यक्तियों की पहचान करने में मदद करेगा
पेम के रूप। हम अपने अध्ययन की शुरुआत मैथमस के लक्षणों और लक्षणों की पहचान करके करते हैं
ଚିହ୍ନ ତେବେ, ଏହି ଫର୍ମଗୁଡ଼ିକ ପରସ୍ପରଠାରୁ କିପରି ଭିନ୍ନ? ନିମ୍ନରେ ବର୍ଣ୍ଣନା
ବିଭିନ୍ନ ପ୍ରକାରର PEM ର ଏକ ସ୍ପଷ୍ଟ ଚିତ୍ର ଉପସ୍ଥାପନ କରେ ଏବଂ ଚିହ୍ନ ଏବଂ ଲକ୍ଷଣଗୁଡିକ ତାଲିକାଭୁକ୍ତ କରେ |
ପ୍ରତ୍ୟେକ ଫର୍ମ ପାଇଁ ନିର୍ଦ୍ଦିଷ୍ଟ, ଯାହା ଆମକୁ ବିଭିନ୍ନ ରୋଗରେ ପୀଡିତ ବ୍ୟକ୍ତିବିଶେଷଙ୍କୁ ଚିହ୍ନଟ କରିବାରେ ସାହାଯ୍ୟ କରିବ |
PEM ର ଫର୍ମ | ମ୍ୟାଟାମସ୍ ର ଲକ୍ଷଣ ଏବଂ ଲକ୍ଷଣ ଚିହ୍ନଟ କରି ଆମେ ଆମର ଅଧ୍ୟୟନ ଆରମ୍ଭ କରୁ |
characterized very low body weight for age, loss of subcutaneous fat (fat under the
skin) gross muscle wasting. It is observed more frequently infants and very young
children, Marasmus is usually due to very severe Causes.
उम्र के लिए बहुत कम शरीर के वजन की विशेषता, चमड़े के नीचे की वसा (के तहत वसा) की हानि
त्वचा) सकल मांसपेशियों को बर्बाद करना। यह अधिक बार शिशुओं और बहुत युवा मनाया जाता है
बच्चों, मैरासमस आमतौर पर बहुत गंभीर कारणों के कारण होता है।
ବୟସ ପାଇଁ ଅତ୍ୟଧିକ କମ୍ ଶରୀରର ଓଜନ, ସବ୍କ୍ୟୁଟାନ୍ସ ଫ୍ୟାଟ୍ ହ୍ରାସ (ବର୍ଣ୍ଣିତ ଚର୍ବି |
ଚର୍ମ) ମୋଟ ମାଂସପେଶୀ ନଷ୍ଟ | ଏହା ବାରମ୍ବାର ଶିଶୁ ଏବଂ ବହୁତ ଛୋଟ ଦେଖାଯାଏ |
ପିଲାମାନେ, ମାରାସମସ୍ ସାଧାରଣତ very ଅତ୍ୟଧିକ ଭୟଙ୍କର କାରଣ ହେତୁ ହୋଇଥାଏ |

of landless agricultural labourers, backward communities and nomadic tribes. These
communities are poor, illiterate and without any regular earnings, therefore, they are
unable to provide enough food for their large families. Children living in urban
slums are also at risk.
भूमिहीन खेतिहर मजदूरों, पिछड़े समुदायों और घुमंतू जनजातियों में। इन
समुदाय गरीब, अनपढ़ और बिना किसी नियमित कमाई के हैं, इसलिए, वे हैं
अपने बड़े परिवारों के लिए पर्याप्त भोजन प्रदान करने में असमर्थ। शहरी में रहने वाले बच्चे
झुग्गियों को भी खतरा है।
ଭୂମିହୀନ କୃଷି ଶ୍ରମିକ, ପଛୁଆ ସମ୍ପ୍ରଦାୟ ଏବଂ ନାମମାତ୍ର ଜନଜାତିର | ଏଗୁଡ଼ିକ |
ସମ୍ପ୍ରଦାୟ ଗରିବ, ଅଶିକ୍ଷିତ ଏବଂ କ regular ଣସି ନିୟମିତ ରୋଜଗାର ବିନା, ତେଣୁ, ସେମାନେ |
ସେମାନଙ୍କର ବଡ଼ ପରିବାର ପାଇଁ ପର୍ଯ୍ୟାପ୍ତ ଖାଦ୍ୟ ଯୋଗାଇବାରେ ଅସମର୍ଥ | ସହରୀରେ ରହୁଥିବା ପିଲାମାନେ |
ums ୁଲା ମଧ୍ୟ ବିପଦରେ ଅଛି |
nutritional status of the mother and its impact on pregnancy? We learnt that the
nutritional status of the mother determines the state of nutrition of the child to be
borm.
If the nutritional status of the mother is poor, the
chances of the offspring being
malnourished are higher. Maternal malnutrition results in low birth weight of
offspring. Infants with birth weight lower than 2500 grams (2.5 kg) are considered as
low birth weight babies. Children who develop PEM often begin life with a low birth
weight
माँ की पोषण स्थिति और गर्भावस्था पर इसका प्रभाव? हमने सीखा कि
मां की पोषण स्थिति बच्चे के पोषण की स्थिति को निर्धारित करती है
borm।
यदि मां की पोषण की स्थिति खराब है, तो
संतान होने की संभावना
कुपोषित अधिक हैं। मातृ कुपोषण के परिणामस्वरूप कम वजन का जन्म होता है
वंश। 2500 ग्राम (2.5 किग्रा) से कम वजन वाले शिशुओं को माना जाता है
कम जन्म के बच्चे। पीईएम विकसित करने वाले बच्चे अक्सर कम जन्म के साथ जीवन शुरू करते हैं
वजन
ମାତାର ପୁଷ୍ଟିକର ସ୍ଥିତି ଏବଂ ଗର୍ଭଧାରଣ ଉପରେ ଏହାର ପ୍ରଭାବ? ଆମେ ଶିଖିଲୁ
ମା’ର ପୁଷ୍ଟିକର ସ୍ଥିତି ଶିଶୁର ପୁଷ୍ଟିକର ସ୍ଥିତି ନିର୍ଣ୍ଣୟ କରେ |
borm।
ଯଦି ମାତାର ପୁଷ୍ଟିକର ସ୍ଥିତି ଖରାପ,
ବଂଶର ସମ୍ଭାବନା |
ପୁଷ୍ଟିହୀନତା ଅଧିକ | ମାତୃ ପୁଷ୍ଟିହୀନତା କମ୍ ଜନ୍ମ ଓଜନରେ ପରିଣତ ହୁଏ |
ବଂଶ ଜନ୍ମ ଓଜନ 2500 ଗ୍ରାମ (2.5 କିଲୋଗ୍ରାମ) ରୁ କମ୍ ଥିବା ଶିଶୁମାନଙ୍କୁ ବିବେଚନା କରାଯାଏ |
କମ୍ ଜନ୍ମ ଓଜନ ଶିଶୁ | ଯେଉଁ ପିଲାମାନେ PEM ର ବିକାଶ କରନ୍ତି ସେମାନେ କମ୍ ଜନ୍ମରୁ ଜୀବନ ଆରମ୍ଭ କରନ୍ତି |
ଓଜନ
(frequent loose motions) or an attack of measles. In the urban slums, in particular,
artificial feeding with commercial milk foods is common. The mothers may follow
unsound and unhygienic methods of feeding the child. Feeding bottles may not be
properly sterilized Flies may be allowed to sit on the nipple of the feeding bottle.
This may lead to frequent diarrhea.
and lead to marasmus. Hence, the importance of
good hygiene is not realized leading to ill-health and malnutrition.
(लगातार लूज मोशन) या खसरे का दौरा। शहरी मलिन बस्तियों में, विशेष रूप से,
वाणिज्यिक दूध खाद्य पदार्थों के साथ कृत्रिम खिला आम है। माताओं का पालन हो सकता है
बच्चे को दूध पिलाने की अस्वाभाविक और अनहेल्दी विधियाँ। दूध पिलाने की बोतलें नहीं हो सकती हैं
ठीक से निष्फल मक्खियों को खिला बोतल के निप्पल पर बैठने की अनुमति दी जा सकती है।
इससे बार-बार दस्त हो सकते हैं।
और marasmus के लिए नेतृत्व। इसलिए, का महत्व
अच्छी स्वच्छता का एहसास स्वास्थ्य और कुपोषण की ओर नहीं होता है।
(ବାରମ୍ବାର ଖାଲି ଗତି) କିମ୍ବା ମିଳିମିଳା ଆକ୍ରମଣ | ସହରୀ ବସ୍ତିରେ, ବିଶେଷ ଭାବରେ,
ବାଣିଜ୍ୟିକ ଦୁଗ୍ଧ ଖାଦ୍ୟ ସହିତ କୃତ୍ରିମ ଖାଇବା ସାଧାରଣ ଅଟେ | ମାତାମାନେ ଅନୁସରଣ କରିପାରନ୍ତି |
ଶିଶୁକୁ ଖାଇବାକୁ ଦେବାର ଅସଂପୂର୍ଣ୍ଣ ଏବଂ ଅପରିଷ୍କାର ପଦ୍ଧତି ବୋତଲ ଖାଇବା ସମ୍ଭବ ନୁହେଁ |
ସଠିକ୍ ଭାବରେ ନିର୍ଜଳିତ ମାଛିମାନଙ୍କୁ ଫିଡିଂ ବୋତଲର ସ୍ତନରେ ବସିବାକୁ ଅନୁମତି ଦିଆଯାଇପାରେ |
ଏହା ବାରମ୍ବାର arr ାଡ଼ା ହୋଇପାରେ |
ଏବଂ ମାରାସମସ୍ ଆଡକୁ ଯାଆନ୍ତୁ | ତେଣୁ, ଏହାର ଗୁରୁତ୍ୱ |
ଉତ୍ତମ ସ୍ ene ଚ୍ଛତା ଅସୁସ୍ଥତା ଏବଂ ପୁଷ୍ଟିହୀନତାର କାରଣ ହୋଇଥାଏ |
mother. You have read about the close relationship between malnutrition and
infection in thit 2 (Block 1) of this course. The mother, due to ignorance delays the
introduction of supplementary food even upto the age of 1 year. This has serious
consequences because mother’s milk alone is not enough for the child By the age of 6
months the infant should given supplement foods in addition breast milk.
Further, in case when the child is suffering from infections such as diarrhoea,
measles and common fevers the mother restricts the diet of the child. This practice is
मां। आपने कुपोषण और के बीच घनिष्ठ संबंध के बारे में पढ़ा है
इस कोर्स के थिट 2 (ब्लॉक 1) में संक्रमण। अज्ञानता के कारण माँ, देरी करती है
1 वर्ष की आयु तक भी पूरक भोजन की शुरूआत। यह गंभीर है
परिणाम क्योंकि माँ का दूध अकेले बच्चे के लिए पर्याप्त नहीं है 6 वर्ष की आयु तक
महीनों के शिशु को स्तन के दूध के अतिरिक्त पूरक आहार देना चाहिए।
इसके अलावा, जब बच्चा डायरिया जैसे संक्रमण से पीड़ित होता है,
माँ का खसरा और आम बुखार बच्चे के आहार को प्रतिबंधित करता है। यह अभ्यास है
इस तरह के आहार प्रतिबंध के बाद से अच्छा नहीं है जो पहले से ही बच्चों में पीईएम की ओर जाता है
अल्पपोषित।
ମା ପୁଷ୍ଟିହୀନତା ମଧ୍ୟରେ ଥିବା ଘନିଷ୍ଠ ସମ୍ପର୍କ ବିଷୟରେ ଆପଣ ପ read ିଛନ୍ତି |
ଏହି ପାଠ୍ୟକ୍ରମର thit 2 (ବ୍ଲକ 1) ରେ ସଂକ୍ରମଣ | ଅଜ୍ଞତା ହେତୁ ମାତା ବିଳମ୍ବ କରନ୍ତି |
1 ବର୍ଷ ବୟସ ପର୍ଯ୍ୟନ୍ତ ସପ୍ଲିମେଣ୍ଟାରୀ ଖାଦ୍ୟର ପରିଚୟ | ଏହାର ଗମ୍ଭୀରତା ଅଛି |
ଏହାର ପରିଣାମ କାରଣ କେବଳ ମା’ର କ୍ଷୀର ପିଲାଙ୍କ ପାଇଁ ପର୍ଯ୍ୟାପ୍ତ ନୁହେଁ 6 ବର୍ଷ ବୟସ ପର୍ଯ୍ୟନ୍ତ |
ମାସ ମାସ ଶିଶୁକୁ ସ୍ତନ୍ୟପାନ ବ୍ୟତୀତ ସପ୍ଲିମେଣ୍ଟ ଖାଦ୍ୟ ଦେବା ଉଚିତ୍ |
ଅଧିକନ୍ତୁ, ଯେତେବେଳେ ଶିଶୁ arr ାଡ଼ା ଭଳି ସଂକ୍ରମଣରେ ପୀଡିତ,
ମିଳିମିଳା ଏବଂ ସାଧାରଣ ଜ୍ୱର ମା ଶିଶୁର ଖାଦ୍ୟକୁ ପ୍ରତିବନ୍ଧିତ କରେ | ଏହି ଅଭ୍ୟାସ ହେଉଛି |
ଭଲ ନୁହେଁ ଯେହେତୁ ଏହିପରି ଖାଦ୍ୟପେୟ ପ୍ରତିବନ୍ଧକ ପିଲାମାନଙ୍କ ମଧ୍ୟରେ PEM କୁ ନେଇଥାଏ |
ଅଣ୍ଡରଫେଡ୍ |
addition to breast milk are introduced quite late. The child is usually given the same
diet taken by adults and very often follow the same meal pattern. The typical Indian
diet is based on cereals and is quite bulky for a small child. This would mean that the
child can consume only smaller amounts of the food at one time.
स्तन के दूध के अलावा काफी देर से पेश किया जाता है। बच्चे को आमतौर पर वही दिया जाता है
वयस्कों द्वारा लिया गया आहार और अक्सर एक ही भोजन पद्धति का पालन करते हैं। ठेठ भारतीय
आहार अनाज पर आधारित है और एक छोटे बच्चे के लिए काफी भारी है। इसका मतलब यह होगा कि ए
बच्चा एक समय में केवल कम मात्रा में भोजन का उपभोग कर सकता है।
ସ୍ତନ୍ୟପାନ ସହିତ ବହୁ ବିଳମ୍ବରେ ପରିଚିତ ହୁଏ | ପିଲାକୁ ସାଧାରଣତ the ସମାନ ଦିଆଯାଏ |
ବୟସ୍କମାନଙ୍କ ଦ୍ taken ାରା ନିଆଯାଇଥିବା ଖାଦ୍ୟ ଏବଂ ପ୍ରାୟତ the ସମାନ ଭୋଜନ ପଦ୍ଧତି ଅନୁସରଣ କରନ୍ତି | ସାଧାରଣ ଭାରତୀୟ |
ଖାଦ୍ୟ ଶସ୍ୟ ଉପରେ ଆଧାରିତ ଏବଂ ଏକ ଛୋଟ ପିଲା ପାଇଁ ଏହା ବହୁତ ବଡ ଅଟେ | ଏହାର ଅର୍ଥ ହେଉଛି
ପିଲା ଏକ ସମୟରେ କେବଳ ଅଳ୍ପ ପରିମାଣର ଖାଦ୍ୟ ଖାଇପାରେ |
health problem in India. Xerophthalmia, refers to the eye manifestations (signs)
arising due to vitamin A deficiency. Blindness, resulting due to xerophthalmia, is a
major health problem. Although vitamin A deficiency may become apparent at all
ages, the preschool child is the most frequent victim of this debilitating disorder.
According to rough estimates thirty thousand to forty thousand children may loose
their eyesight due to vitamin deficiency in India.
भारत में स्वास्थ्य समस्या। ज़ेरोफथाल्मिया, आंखों की अभिव्यक्तियों (संकेत) को संदर्भित करता है
विटामिन ए की कमी के कारण उत्पन्न होना। अंधापन, जिसके परिणामस्वरूप जेरोफथाल्मिया है, ए
प्रमुख स्वास्थ्य समस्या। हालांकि विटामिन ए की कमी बिल्कुल स्पष्ट हो सकती है
उम्र, पूर्वस्कूली बच्चा इस दुर्बलता विकार का सबसे लगातार शिकार है।
मोटे अनुमान के अनुसार तीस हजार से चालीस हजार बच्चे ढीले हो सकते हैं
भारत में विटामिन की कमी के कारण उनकी आंखों की रोशनी चली गई।
ଭାରତରେ ସ୍ୱାସ୍ଥ୍ୟ ସମସ୍ୟା | ଜେରୋଫଥାଲମିଆ, ଆଖିର ପ୍ରକାଶ (ଚିହ୍ନ) କୁ ବୁ .ାଏ |
ଭିଟାମିନ୍ ଏ ଅଭାବ ହେତୁ ଉତ୍ପନ୍ନ | ଜେରୋଫଥାଲମିଆ ହେତୁ ଅନ୍ଧତା ହେଉଛି |
ପ୍ରମୁଖ ସ୍ୱାସ୍ଥ୍ୟ ସମସ୍ୟା | ଯଦିଓ ଭିଟାମିନ୍ ଏ ଅଭାବ ଆଦ appar ସ୍ପଷ୍ଟ ହୋଇପାରେ |
ବୟସ, ପ୍ରାଥମିକ ବିଦ୍ୟାଳୟର ପିଲା ଏହି ଦୁର୍ବଳ ବ୍ୟାଧିର ବାରମ୍ବାର ଶିକାର ହୁଅନ୍ତି |
ପାଖାପାଖି ଆକଳନ ଅନୁଯାୟୀ ତିରିଶ ହଜାରରୁ ଚାଳିଶ ହଜାର ପିଲା ଖାଲି ହୋଇପାରନ୍ତି |
ଭାରତରେ ଭିଟାମିନ୍ ଅଭାବ ହେତୁ ସେମାନଙ୍କର ଦୃଷ୍ଟି ଶକ୍ତି |
What are the signs and symptoms of this disorder? On reading through this section
you will be introduced to the various eye changes (clinical features) common to
Vitamin A deficiency.
इस विकार के लक्षण और लक्षण क्या हैं? इस खंड के माध्यम से पढ़ने पर
आपको विभिन्न नेत्र परिवर्तनों (नैदानिक सुविधाओं) से परिचित कराया जाएगा
विटामिन ए की कमी।
ଏହି ବିକୃତିର ଲକ୍ଷଣ ଏବଂ ଲକ୍ଷଣଗୁଡ଼ିକ କ’ଣ? ଏହି ବିଭାଗ ମାଧ୍ୟମରେ ପ On ିବା ଉପରେ |
ଆପଣ ସାଧାରଣ ଆଖି ପରିବର୍ତ୍ତନ (କ୍ଲିନିକାଲ୍ ବ features ଶିଷ୍ଟ୍ୟ) ସହିତ ପରିଚିତ ହେବେ |
ଭିଟାମିନ୍ ଏ ଅଭାବ |

pertain to changes in the eye.
आंख में परिवर्तन से संबंधित है।
ଆଖିରେ ପରିବର୍ତ୍ତନ ସମ୍ବନ୍ଧୀୟ |
:max_bytes(150000):strip_icc()/GettyImages-695204442-b9320f82932c49bcac765167b95f4af6.jpg)
eye. It is the conjunctiva (thin transparent membrane that covers the cornea and lines
the inside of the eyelid) and the cornea (the anterior, transparent portion of the
outermost layer of the eye) which are most often affected by the deficiency.
आँख। यह कंजाक्तिवा (पतली पारदर्शी झिल्ली) है जो कॉर्निया और रेखाओं को कवर करती है
पलक के अंदर) और कॉर्निया (पूर्वकाल, पारदर्शी भाग)
आंख की सबसे बाहरी परत) जो अक्सर कमी से प्रभावित होती है।
ଆଖି ଏହା ହେଉଛି କଞ୍ଜୁକ୍ଟିଭା (ପତଳା ସ୍ୱଚ୍ଛ ମେମ୍ବ୍ରେନ୍ ଯାହା କର୍ଣ୍ଣିଆ ଏବଂ ରେଖାଗୁଡ଼ିକୁ ଆବୃତ କରେ |
ଆଖିର ଭିତର) ଏବଂ କର୍ଣ୍ଣିଆ (ପୂର୍ବ, ସ୍ୱଚ୍ଛ ଅଂଶ |
ଆଖିର ବାହ୍ୟ ସ୍ତର) ଯାହା ପ୍ରାୟତ the ଅଭାବ ଦ୍ୱାରା ପ୍ରଭାବିତ ହୋଇଥାଏ |
in rural areas and urban slums. In India, the disease is more common among the
poorer sections of the community. Vitamin A deficiency may become apparent at all
ages, But, the most common predominantly nutritional, variety occurs in the third
and fourth years of life, at least in countries where breast feeding is prolonged. The
younger the child, the more serious the knife stations and the greater the mortality
rate. The cornea is rarely affected in children beyond the age of five years. In fact, the
prevalence of corneal xerophthalmia is maximum between the ages of 1 and 3 years,
The disease is relatively more frequent among males.
ग्रामीण क्षेत्रों और शहरी मलिन बस्तियों में। भारत में, यह बीमारी अधिक आम है
समुदाय के गरीब वर्ग। विटामिन ए की कमी बिल्कुल स्पष्ट हो सकती है
उम्र, लेकिन, सबसे आम मुख्य रूप से पोषण, विविधता तीसरे में होती है
और जीवन के चौथे वर्ष, कम से कम उन देशों में जहां स्तन पान करना लम्बा है।
छोटे बच्चे, चाकू स्टेशनों और अधिक गंभीर मृत्यु दर
मूल्यांकन करें। पांच साल से अधिक उम्र के बच्चों में कॉर्निया शायद ही कभी प्रभावित होता है। वास्तव में,
कॉर्नियल ज़ेरोफथाल्मिया की व्यापकता 1 और 3 वर्ष की आयु के बीच अधिकतम है,
यह बीमारी पुरुषों में अपेक्षाकृत अधिक होती है।
ଗ୍ରାମାଞ୍ଚଳ ଏବଂ ସହରୀ ବସ୍ତିରେ | ଭାରତରେ ଏହି ରୋଗ ଅଧିକ ଦେଖାଯାଏ
ସମ୍ପ୍ରଦାୟର ଗରିବ ବିଭାଗ | ଭିଟାମିନ୍ ଏ ଅଭାବ ଆଦ appar ସ୍ପଷ୍ଟ ହୋଇପାରେ |
ବୟସ, କିନ୍ତୁ, ସାଧାରଣତ nut ପୁଷ୍ଟିକର, ତୃତୀୟରେ ବିଭିନ୍ନତା ଦେଖାଯାଏ |
ଏବଂ ଜୀବନର ଚତୁର୍ଥ ବର୍ଷ, ଅନ୍ତତ least ପକ୍ଷେ ଯେଉଁ ଦେଶରେ ସ୍ତନ୍ୟପାନ ଦୀର୍ଘସ୍ଥାୟୀ ହୁଏ | େଯମାେନ
ଛୋଟ ପିଲା, ଛୁରୀ ଷ୍ଟେସନ ଯେତେ ଗମ୍ଭୀର ଏବଂ ମୃତ୍ୟୁହାର ଅଧିକ |
ହାର ପାଞ୍ଚ ବର୍ଷରୁ ଅଧିକ ପିଲାମାନଙ୍କଠାରେ କର୍ଣ୍ଣିଆ କ୍ୱଚିତ୍ ପ୍ରଭାବିତ ହୁଏ | ବାସ୍ତବରେ,
କର୍ନିଆଲ୍ ଜେରୋଫଥାଲମିଆର ପ୍ରାଦୁର୍ଭାବ 1 ରୁ 3 ବର୍ଷ ମଧ୍ୟରେ ସର୍ବାଧିକ,
ଏହି ରୋଗ ପୁରୁଷମାନଙ୍କ ମଧ୍ୟରେ ଅପେକ୍ଷାକୃତ ଅଧିକ ହୋଇଥାଏ |
low liver stores of vitamin A because their mothers are also deficient in vitamin A
have low vitamin A reserves in the body. vitamin A is fat-soluble and can be stored in the body for longer
periods
विटामिन ए के कम जिगर भंडार क्योंकि उनकी माताओं को भी विटामिन ए की कमी होती है
गर्भावस्था के दौरान महिलाएं बहुत कम मात्रा में विटामिन ए का सेवन करती रहती हैं
या तो गरीबी या अज्ञानता के कारण। परिणामस्वरूप, ऐसी महिलाओं के लिए बच्चे पैदा हुए
शरीर में कम विटामिन ए का भंडार है। विटामिन ए वसा में घुलनशील है और इसे लंबे समय तक शरीर में संग्रहीत किया जा सकता है
अवधि
ଭିଟାମିନ୍ ଏ ର କମ୍ ଯକୃତ ଷ୍ଟୋର୍, କାରଣ ସେମାନଙ୍କ ମା’ମାନେ ମଧ୍ୟ ଭିଟାମିନ୍ ଏରେ ଅଭାବ |
ଗର୍ଭାବସ୍ଥାରେ ମହିଳାମାନେ ବହୁତ କମ୍ ପରିମାଣର ଭିଟାମିନ୍ ଏ ଖାଇବା ଜାରି ରଖନ୍ତି |
ଦାରିଦ୍ରତା କିମ୍ବା ଅଜ୍ଞତା ହେତୁ | ଫଳସ୍ୱରୂପ, ଏହିପରି ମହିଳାମାନଙ୍କ ପାଇଁ ଜନ୍ମ ହୋଇଥିବା ପିଲାମାନେ |
ଶରୀରରେ ଭିଟାମିନ୍ ଏ ଭଣ୍ଡାର କମ୍ ଥାଏ | ଭିଟାମିନ୍ ଏ ଚର୍ବିରେ ଦ୍ରବୀଭୂତ ଏବଂ ଶରୀରରେ ଅଧିକ ସମୟ ଗଚ୍ଛିତ ହୋଇପାରେ |
ଅବଧିଗୁଡିକ
inadequacy of vitamin A. In the villages and urban slums, among the low income
groups, the intake of vitamin A is less than a quarter of the Recommended Dietary
intakes (RDI). As long as the child is breast fed, the vitamin A status of the infants is
apparently adequate because the infant gets reasonable amounts of vitamin A
through breast milk. Once the child is taken off the breast, the child is put on the
family diet which is deficient in vitamin A. Due to ii adequate consumption of
vitamin A, the child develops vitamin A deficiency manifesting as xerophthalmia.
कम आय के बीच गांवों और शहरी झुग्गियों में विटामिन ए की अपर्याप्तता
समूह, विटामिन ए का सेवन अनुशंसित आहार के एक चौथाई से भी कम है
intakes (RDI)। जब तक बच्चा स्तनपान करता है, तब तक शिशुओं की विटामिन ए स्थिति होती है
स्पष्ट रूप से पर्याप्त है क्योंकि शिशु को उचित मात्रा में विटामिन ए मिलता है
स्तन के दूध के माध्यम से। एक बार जब बच्चे को स्तन से निकाल दिया जाता है, तो बच्चे को डाल दिया जाता है
पारिवारिक आहार जिसमें विटामिन ए की कमी होती है। ii के पर्याप्त सेवन के कारण
विटामिन ए, बच्चे में विटामिन ए की कमी से विकसित होता है जो कि ज़ेरोफथाल्मिया के रूप में प्रकट होता है।
ଭିଟାମିନ୍ ଏ ର ଅପାରଗତା କମ୍ ଆୟ ମଧ୍ୟରେ ଗାଁ ଏବଂ ସହରାଞ୍ଚଳ ବସ୍ତିରେ |
ଗୋଷ୍ଠୀ, ଭିଟାମିନ୍ ଏ ଗ୍ରହଣ କରିବା ସୁପାରିଶ କରାଯାଇଥିବା ଖାଦ୍ୟର ଏକ ଚତୁର୍ଥାଂଶରୁ କମ୍ ଅଟେ |
ଭୋଜନ (RDI) | ଯେପର୍ଯ୍ୟନ୍ତ ଶିଶୁକୁ ସ୍ତନ୍ୟପାନ କରାଏ, ଶିଶୁମାନଙ୍କର ଭିଟାମିନ୍ ଏ ସ୍ଥିତି ଥାଏ |
ବୋଧହୁଏ ପର୍ଯ୍ୟାପ୍ତ କାରଣ ଶିଶୁଟି ଯଥେଷ୍ଟ ପରିମାଣର ଭିଟାମିନ୍ ଏ ପାଇଥାଏ |
ସ୍ତନ୍ୟପାନ ମାଧ୍ୟମରେ ଥରେ ଶିଶୁକୁ ସ୍ତନରୁ ବାହାର କରିଦେଲେ, ପିଲାଟି ଉପରେ ରଖାଯାଏ |
ପାରିବାରିକ ଖାଦ୍ୟ ଯାହାକି ଭିଟାମିନ୍ ଏରେ ଅଭାବ | ii ପର୍ଯ୍ୟାପ୍ତ ପରିମାଣର ବ୍ୟବହାର ହେତୁ |
ଭିଟାମିନ୍ ଏ, ପିଲାଟି ଭିଟାମିନ୍ ଏ ଅଭାବର ବିକାଶ କରେ ଯାହା ଜେରୋଫଥାଲମିଆ ଭାବରେ ଦେଖାଯାଏ |
infestations like round worm disease are very common in young children. These are
known to decrease the absorption of vitamin A and lead to its deficiency. Measles,
one of the childhood infections, is another important cause of xerophthalmia leading
particularly to corneal sores and blindness. Few of the most common causes of
xerophthalmia have been discussed above. What preventive measures and treatment
can be prescribed to overcome this disorder is the next point of discussion
छोटे बच्चों में गोल कृमि रोग जैसे संक्रमण बहुत आम हैं। य़े हैं
विटामिन ए के अवशोषण को कम करने और इसकी कमी का नेतृत्व करने के लिए जाना जाता है। खसरा,
बचपन के संक्रमणों में से एक, जेरोफथाल्मिया अग्रणी का एक और महत्वपूर्ण कारण है
विशेष रूप से कॉर्नियल घावों और अंधापन। के सबसे आम कारणों में से कुछ
ऊपर जेरोफथाल्मिया की चर्चा की गई है। क्या निवारक उपाय और उपचार
इस विकार को दूर करने के लिए निर्धारित किया जा सकता है चर्चा का अगला बिंदु है
ଛୋଟ ପିଲାମାନଙ୍କଠାରେ ଗୋଲାକାର ପୋକ ରୋଗ ପରି ସଂକ୍ରମଣ ଅତି ସାଧାରଣ ଅଟେ | ଏହି ସବୁ
ଭିଟାମିନ୍ ଏ ର ଅବଶୋଷଣ ହ୍ରାସ କରିବା ଏବଂ ଏହାର ଅଭାବକୁ ଜଣା | ମିଳିମିଳା,
ପିଲାଦିନର ସଂକ୍ରମଣ ମଧ୍ୟରୁ ଜେରୋଫଥାଲମିଆର ଅନ୍ୟ ଏକ ଗୁରୁତ୍ୱପୂର୍ଣ୍ଣ କାରଣ |
ବିଶେଷକରି କର୍ନିଆ ଘା ’ଏବଂ ଅନ୍ଧତା ପାଇଁ | ଏହାର ସାଧାରଣ କାରଣଗୁଡ଼ିକ ମଧ୍ୟରୁ ଅଳ୍ପ କିଛି |
ଜେରୋଫଥାଲମିଆ ଉପରେ ଆଲୋଚନା କରାଯାଇଛି | କ’ଣ ପ୍ରତିଷେଧକ ବ୍ୟବସ୍ଥା ଏବଂ ଚିକିତ୍ସା |
ଏହି ବିଶୃଙ୍ଖଳାକୁ ଦୂର କରିବା ପାଇଁ ପରବର୍ତ୍ତୀ ଆଲୋଚନା ହେଉଛି |
a nutritional deficiency occurring due to reduced intakes of riboflavin through the
diet. Riboflavin deficiency is one of the most common among the B-complex
deficiencies. How do we detect that a person is suffering from riboflavin deficiency?
As in the case of other deficiency diseases, this disease is also associated with certain
obvious clinical features. Let us consider these features.
के माध्यम से राइबोफ्लेविन के कम इंटेक के कारण होने वाली पोषण संबंधी कमी
आहार। राइबोफ्लेविन की कमी बी-कॉम्प्लेक्स में सबसे आम में से एक है
कमियों। हम कैसे पता लगाते हैं कि एक व्यक्ति राइबोफ्लेविन की कमी से पीड़ित है?
जैसा कि अन्य कमी रोगों के मामले में होता है, यह रोग भी निश्चित रूप से जुड़ा होता है
स्पष्ट नैदानिक विशेषताएं। आइए हम इन विशेषताओं पर विचार करें।
which are the rich food sources of riboflavin? Green leafy vegetables, milk, organ
meats are good sources of riboflavin. Whole grain cereals, pulses, nuts provide
riboflavin in moderate amounts. In the families of poor rural communities, diets
contain negligible amounts of pulses and milk. Meat may be consumed, but very
rarely. As a result, riboflavin deficiency is very common in our country. You have
also learnt that Indian diets are mainly cereal(ଶସ୍ୟ) based. Cereals are not good sources of
riboflavin. Therefore, our diets tend to be deficient in riboflavin
राइबोफ्लेविन के समृद्ध खाद्य स्रोत कौन से हैं? हरी पत्तेदार सब्जियां, दूध, अंग
मीट राइबोफ्लेविन के अच्छे स्रोत हैं। साबुत अनाज अनाज, दालें, नट प्रदान करते हैं
मध्यम मात्रा में राइबोफ्लेविन। गरीब ग्रामीण समुदायों के परिवारों में, आहार
दालों और दूध की नगण्य मात्रा में होते हैं। मांस का सेवन किया जा सकता है, लेकिन बहुत
शायद ही कभी। परिणामस्वरूप, हमारे देश में राइबोफ्लेविन की कमी बहुत आम है। आपके पास
यह भी सीखा कि भारतीय आहार मुख्य रूप से अनाज (based) आधारित हैं। अनाज अच्छे स्रोत नहीं हैं
राइबोफ्लेविन। इसलिए, हमारे आहार में राइबोफ्लेविन की कमी होती है
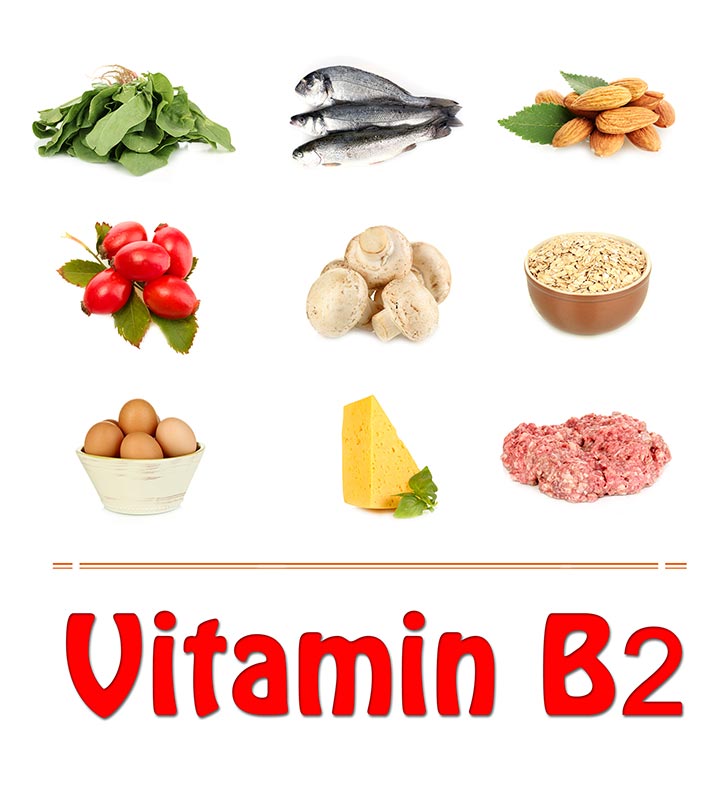
Vitamin. One tablet of B-complex daily for about one week to ten days, will help
treat the deficiency.
विटामिन। लगभग एक सप्ताह से दस दिनों तक रोजाना बी-कॉम्प्लेक्स की एक गोली, मदद करेगी
कमी का इलाज करें।

cannot afford milk, in view of its high cost. We have to, therefore, make sure that
people include other rich food sources of riboflavin such as green leafy vegetables,
whole cereals and pulses and cheaper nut in their every day diet to prevent
ariboflavinosis.
इसकी उच्च लागत को देखते हुए दूध नहीं दे सकते। इसलिए हमें यह सुनिश्चित करना होगा
लोगों में राइबोफ्लेविन के अन्य समृद्ध खाद्य स्रोत शामिल हैं जैसे हरी पत्तेदार सब्जियां,
पूरे अनाज और दालों और अपने दैनिक आहार में सस्ता अखरोट को रोकने के लिए
ariboflavinosis।
vitamin called thiamine(vitamin B1) in the diet. It is interesting to note that thiamine deficiency is rare in our
country
आहार में विटामिन जिसे थायमिन (विटामिन बी 1) कहा जाता है। यह ध्यान रखना दिलचस्प है कि थियामिन की कमी हमारे यहां दुर्लभ है
देश
start with, experiences loss of appetite, weakness and heaviness in the legs. The
person also becomes tired easily.
The patient complains of the feeling of pins and needles and numbness in the legs.
There may be loss of sensation i.e. loss of the feeling of touch over the legs. The
disease occurs in two forms. It manifests itself either as wet beriberi or dry beriberi.
Wet beriberi is characterized by accumulation of fluid in the body. This can
ultimately lead to heart failure. The patient may complain of palpitation (forcible
and rapid heart beats felt by the patient) and sometimes of chest pain. There may
also be pain in the leg muscles on application of pressure.
शुरुआत करें, पैरों में भूख की कमी, कमजोरी और भारीपन का अनुभव करें।
व्यक्ति भी आसानी से थक जाता है।
रोगी को पिंस और सुइयों की भावना और पैरों में सुन्नता की शिकायत होती है।
सनसनी का नुकसान हो सकता है यानी पैरों पर स्पर्श की भावना का नुकसान।
रोग दो रूपों में होता है। यह या तो गीली बेरीबेरी या सूखी बेरीबेरी के रूप में प्रकट होता है।
गीला बेरीबेरी शरीर में तरल पदार्थ के संचय की विशेषता है। यह हो सकता है
अंतत: हृदय गति रुक जाती है। रोगी को तालुमूल (जबरन) की शिकायत हो सकती है
और रोगी को तेज धड़कन महसूस होती है) और कभी-कभी छाती में दर्द भी होता है। वहाँ हो सकता है
दबाव के आवेदन पर पैर की मांसपेशियों में भी दर्द होना।

making the patient completely bed-ridden
disease is very common in communities consuming rice which is highly polished.
What happens during polishing? During polishing the thin outer layer of rice (which
contains thiamine) is removed. In parts of South India, beriberi was commonly seen
when highly polished rice was being consumed. It is rare in our country now-a-days,
perhaps, because the diets are not based on highly polished rice. Also, rice is rarely
the only staple being consumed. Other cereals are also eaten in varying amounts.
Even in South India, the communities consume diets consisting of wheat, millets
and pulses, though in small amount. These are good sources of thiamine. In the
communities subsisting on parboiled rice, beriberi is not seen.
injection. The patient should be advised complete rest. Thereafter, thiamine tablets
should be given
चावल का सेवन करने वाले समुदायों में बीमारी बहुत आम है जो अत्यधिक पॉलिश है।
पॉलिश करने के दौरान क्या होता है? चावल की पतली बाहरी परत को चमकाने के दौरान (जो कि
थायमिन होता है) को हटा दिया जाता है। दक्षिण भारत के कुछ हिस्सों में, बेरीबेरी आमतौर पर देखा जाता था
जब अत्यधिक पॉलिश किए गए चावल का सेवन किया जा रहा था। हमारे देश में यह अब दुर्लभ है,
शायद, क्योंकि आहार अत्यधिक पॉलिश चावल पर आधारित नहीं हैं। इसके अलावा, चावल शायद ही कभी होता है
केवल मुख्य उपभोग किया जा रहा है। अन्य अनाज भी अलग-अलग मात्रा में खाए जाते हैं।
यहां तक कि दक्षिण भारत में, समुदाय गेहूं, बाजरा से बने आहार का सेवन करते हैं
और दालें, हालांकि कम मात्रा में। ये थायमिन के अच्छे स्रोत हैं। में
पैराइज्ड चावल, बेरीबेरी पर उपस्तिथ समुदायों को नहीं देखा जाता है।
उपचार: गीले और सूखे बेरीबेरी दोनों के मामले में, थायमिन द्वारा दिया जाना चाहिए
इंजेक्शन। रोगी को पूर्ण आराम की सलाह दी जानी चाहिए। इसके बाद, थियामिन की गोलियां
दी जानी चाहिए

polished. In fact, hand pounded rice is the best. We can also take steps to reduce
polishing of rice while milling This will help to prevent loss of thiamine. Further
increase in consumption of thiamine-containing foods should prevent beriberi. The
richest dietary sources of thiamine are yeast and bran (outer layer) of wheat and
millets.
पॉलिश। वास्तव में, हाथ से तैयार चावल सबसे अच्छा है। हम भी कम करने के लिए कदम उठा सकते हैं
मिलिंग के दौरान चावल की पॉलिशिंग यह थायमिन के नुकसान को रोकने में मदद करेगी। आगे की
थायमिन युक्त खाद्य पदार्थों की खपत में वृद्धि को बेरीबेरी को रोकना चाहिए।
थियामिन के सबसे समृद्ध आहार स्रोत गेहूं के खमीर और चोकर (बाहरी परत) हैं
बाजरा।
Rickets is a disease of growing children in which the bones become softened and
deformed due to the deficiency of vitamin D. Osteomalacia, is the adult form of vitamin
D deficiency. In the subsequent discussion we will explore the major features of these
disorders as well as their treatment and prevention. We begin with the causes.
रिकेट्स बढ़ते बच्चों की एक बीमारी है जिसमें हड्डियां नरम हो जाती हैं और
विटामिन डी। ऑस्टियोमलेशिया की कमी के कारण विकृत, विटामिन का वयस्क रूप है
डी की कमी। बाद की चर्चा में हम इनमें से प्रमुख विशेषताओं का पता लगाएंगे
विकारों के साथ ही उनके उपचार और रोकथाम। हम कारणों से शुरू करते हैं।



our country and hence the disease is not as common. However, the disease is more
frequently seen when there is not enough exposure to sunlight. The disease can also
occur when mothers, infants and toddlers receive inadequate vitamin D, either as
food or as supplement. In the subsequent discussion on clinical features, treatment
and prevention we will have to talk about rickets and osteomalacia separately. Let us
begin with rickets.
आपने अद्भुत तथ्य पाया कि विटामिन डी संश्लेषित (निर्मित) है
धूप के संपर्क में आने के बाद त्वचा में। हमारे पास धूप बहुत है
हमारा देश और इसलिए यह बीमारी आम नहीं है। हालांकि, बीमारी अधिक है
अक्सर देखा जाता है जब सूर्य के प्रकाश के पर्याप्त संपर्क नहीं होता है। बीमारी भी हो सकती है
तब होता है जब माताओं, शिशुओं और बच्चों को या तो अपर्याप्त विटामिन डी प्राप्त होता है
भोजन या पूरक के रूप में। नैदानिक सुविधाओं पर बाद की चर्चा में, उपचार
और रोकथाम के लिए हमें रिकेट्स और ओस्टोमैलेशिया के बारे में अलग से बात करनी होगी। हमें करने दो
रिकेट्स के साथ शुरुआत करें।
younger infants in the first six months of life. It is characterized by a range of specific
clinical features as you will see in the following discussion.
जीवन के पहले छह महीनों में छोटे शिशु। यह विशिष्ट की एक श्रृंखला की विशेषता है
नैदानिक विशेषताएं जैसा कि आप निम्नलिखित चर्चा में देखेंगे।
muscles lose their firmness and become flabby. When the abdominal muscles lose
their firmness, the abdomen gets distended. You know that a normal baby’s teeth
erupt at a b particular age. The baby sits and crawls at a particular
age. These are known as development milestones . In
the case of rickets, there is a delay in the physical and motor milestones. For
example, teeth erupt late in children with rickets. There is also considerable delay in
the age at which the child can sit and crawl. The child is too weak and is unable to
walk in some cases. The most important changes caused by this disorder are seen in
the bones. The growing ends of the long bones (like those of the forearm) get
extended and widened. For example there will be a swelling of the forearm bones at
the wrist. There may also be swelling at the ends of the ribs which gives an
appearance of “beading” of ribs. In normal children the opening between the skull
bones closes by about 18 months of age. In rickets the closure of the skull bone is
delayed leading to skull deformation.
chest with the breast bone becoming prominent are common. This protruding of the
breast bone is usually known as pigeon chest. The typical deformities seen in
children who have recovered from rickets are due to the ‘child’s weight bearing
down on the legs before complete recovery takes place. At this time the bones are
still soft and cannot stand the weight of the child. As a result, the children may have
“bow legs” (bent like a bow) or “knock knees” when both the knees will be touching
each other . Deformities of the backbone may also
develop if the disease continues beyond the age of 2 years.
मांसपेशियां अपनी दृढ़ता खो देती हैं और परतदार हो जाती हैं। जब पेट की मांसपेशियां खो जाती हैं
उनकी दृढ़ता, पेट विकृत हो जाता है। आप जानते हैं कि एक सामान्य बच्चे के दांत
एक विशेष उम्र में विस्फोट बच्चा बैठता है और एक विशेष रूप से क्रॉल करता है
उम्र। इन्हें विकास मील के पत्थर के रूप में जाना जाता है। में
रिकेट्स के मामले में, भौतिक और मोटर मील के पत्थर में देरी होती है। के लिये
उदाहरण के लिए, दांत बच्चों के साथ देर से फटते हैं। में भी काफी देरी हुई है
जिस उम्र में बच्चा बैठकर क्रॉल कर सकता है। बच्चा बहुत कमजोर है और असमर्थ है
कुछ मामलों में चलें। इस विकार के कारण सबसे महत्वपूर्ण परिवर्तन देखे गए हैं
हड्डियों। लंबी हड्डियों के बढ़ते छोर (जैसे कि अग्र-भुजाओं के) मिलते हैं
विस्तारित और चौड़ा। उदाहरण के लिए वहाँ पर प्रकोष्ठ की हड्डियों की सूजन होगी
कलाई। पसलियों के छोर पर सूजन भी हो सकती है जो ए देती है
पसलियों के “बीडिंग” की उपस्थिति। सामान्य बच्चों में खोपड़ी के बीच उद्घाटन
हड्डियां लगभग 18 महीने की उम्र तक बंद हो जाती हैं। रिकेट्स में खोपड़ी की हड्डी का बंद होना है
देरी खोपड़ी विरूपण के लिए अग्रणी।
बच्चा अंततः हड्डियों के विभिन्न विकृति विकसित करता है। की विकृति
स्तन की हड्डी के प्रमुख होने के साथ छाती आम हैं। के इस फैलाव
स्तन की हड्डी को आमतौर पर कबूतर की छाती के रूप में जाना जाता है। में देखी गई विशिष्ट विकृति
बच्चे जो रिकेट्स से उबर चुके हैं, वे ‘बच्चे के वजन के कारण’ हैं
पूरी तरह से ठीक होने से पहले पैरों के नीचे। इस समय हड्डियाँ हैं
अभी भी नरम है और बच्चे के वजन को बर्दाश्त नहीं कर सकता। परिणामस्वरूप, बच्चे हो सकते हैं
“धनुष पैर” (धनुष की तरह झुकना) या “घुटनों को मोड़ना” जब दोनों घुटने स्पर्श करेंगे
एक दूसरे । रीढ़ की विकृति भी हो सकती है
यदि रोग 2 वर्ष की आयु से परे जारी है।
requirements for treating rickets. Several preparations of vitamin D are available.
Generally, cure results with daily treatment of vitamin D for about 4 weeks. The
treatment should be supplemented with calcium.
रिकेट्स के इलाज के लिए आवश्यकताएं। विटामिन डी की कई तैयारियाँ उपलब्ध हैं।
आम तौर पर, लगभग 4 सप्ताह के लिए विटामिन डी के दैनिक उपचार के साथ परिणाम ठीक हो जाते हैं।
उपचार कैल्शियम के साथ पूरक होना चाहिए।
the child from rickets. Dietary sources are few and the vitamin is found chiefly in
liver, egg yolk, milk and milk fat (butter and ghee) obtained from animals fed on
pastures exposed to sunlight. Inclusion of these foodstuffs in daily diets prevents
rickets. Supplementation with vitamin D is generally not required in India.
oil is of known value in the prevention of the disease.
बच्चा रिकेट्स से। आहार स्रोत कम हैं और विटामिन मुख्य रूप से पाया जाता है
यकृत, अंडे की ज़र्दी, दूध और दूध की चर्बी (मक्खन और घी) जानवरों को खिलाया जाता है
चरागाहें धूप के संपर्क में। दैनिक आहार में इन खाद्य पदार्थों को शामिल करने से रोकता है
रिकेट्स। भारत में आमतौर पर विटामिन डी के साथ पूरक की आवश्यकता नहीं होती है।
तेल रोग की रोकथाम में ज्ञात मूल्य का है।
challenges faced in the Mid-Day Meal Program.
मध्याह्न भोजन कार्यक्रम में चुनौतियों का सामना करना पड़ा।
Ans, Tamil Nadu was the first to initiate a massive noon meal programme to
children. Neither a child that is hungry, nor a child that is ill can be expected to
learn. Realizing this need the Mid-Day Meal (MDM) Scheme was launched in
primary schools during 1962-63.
The Central Government supplies the full requirement of food grains for the
programme free of cost. For its implementation in rural areas, Panchayats and
Nagarpalikas are also involved or setting up of necessary infrastructure for
preparing cooked food. For this purpose NGOs, women’s group and parent-teacher
councils can be utilized. The total charges for cooking, supervision and kitchen are
eligible for assistance under Poverty Alleviation Programme. In several states,
supplementary feeding was assisted by food supplies from Cooperation for
American Relief Everywhere (CARE) and World Food Programme (WFP). There are
problems of administration and quality of food that have affected the programme
outcomes.
1. Improving the nutritional status of children in classes I – VIII in Government,
Local Body and Government aided schools, and EGS and ATE centers
2. Encouraging poor children, belonging to disadvantaged sections, to attend
school more regularly and help them concentrate on classroom activities.
3. Providing nutritional support to children of primary stage in drought-affected
areas.
implemented in India since August 15, 1995, as a part of the National Program of
Nutritional Support to Primary Education. It was introduced in India with an
objective to enhance enrolment retention and attendance and simultaneously
improving nutritional levels among children. Teachers play a key role in the
successful implementation of mid-day meal scheme at school level. The paper
focuses on the problems faced by teachers in the implementation of mid-day meal
scheme. The study on which this paper is based was conducted in the Jammu
Province. Survey method of descriptive research was used. Multistage sampling
technique was used for the selection of sample. The sample size comprised 200
prepared questionnaire was used to collect the primary data Data was analyzed
using simple statistical technique such as percentages. Teachers pointed out a
number of problems such as problem of management of the mid day meal wastage
of food by the students insufficient and delayed receipt of funds increased
workload of teachers, procuring dry ration from the retail shops lack of
infrastructure for storage cooking and serving food lack of safety provisions
unhygienic surroundings etc being faced by them in implementation of Mid-Day
Meal Scheme. The paper puts forward certain suggestions for effective
implementation of the scheme so that objectives of mid-day meal can be achieved
Ans. During the last four decades, since the attainment of Independence
considerable progress has been achieved in India in the promotion of the health
status of its population. You know that small pox has been completely eliminated,
the expectancy of life at birth has increased significantly. This progress could be
achieved due to several steps taken by the National Government.
Among such measures, one is implementation of a number of health programs.
These programmes are normally referred to as National Health Programmes. Are
you aware of these programmes? For your information, the main health
programmes are listed here:
National Irnmunisation Programme
National Family Welfare Programme
National Programme for Prevention of Nutritional Blindness due to Vitamin A Deficiency
National Nutritional Anaemia Control Programme
National lodine Deficiency Disorders Control Programme
National Filaria Control Programme
National Programme for Control of Blindness
National Aids Control Programme
National Mental Health Programme
National Diabetes Control Programme
National Tuberculosis Control Programme
National Malaria Eradication Programme
Child Survival and Safe Motherhood Programme.
of these programmes are assisted by international health agencies such as WHO and
UNICEF.
Ans. Whatever the child’s lines, you must first make the child comfortable. Try to
reduce the child’s distress and make her rest. The general rules for treating any child
who sick are:
1) Never leave the child alone in a room. Tell the mother or older sibling to stay with
the child and talk to her. If the child is not too sick, an older sibling or friend can
play with her.
2) See that the room is well ventilated. There should not be any draught, but at the
same time there should be fresh air.
3) The child’s clothes and bed clothes should be light and clean, preferably of cotton
Warm clothes, if necessary, should be used over the cotton clothes.
4) Give plenty of liquids to the child to drink to prevent dehydration. If the child has
high fever and/or is breathing rapidly, this will add to dehydration..
5) There should be no strong smells in the room.
बच्चे के संकट को कम करें और उसे आराम दें। किसी भी बच्चे के इलाज के लिए सामान्य नियम
कौन बीमार हैं:
1) बच्चे को कभी भी एक कमरे में अकेला न छोड़ें। मां या बड़ी बहन को साथ रहने के लिए कहें
बच्चे और उससे बात करें। यदि बच्चा बहुत बीमार नहीं है, तो एक बड़ा भाई या दोस्त कर सकता है
उसके साथ खेलें।
2) देखें कि कमरा अच्छी तरह हवादार है। कोई मसौदा नहीं होना चाहिए, लेकिन
उसी समय ताजी हवा होनी चाहिए।
3) बच्चे के कपड़े और बिस्तर के कपड़े हल्के और साफ होने चाहिए, अधिमानतः कपास के
गर्म कपड़े, यदि आवश्यक हो, सूती कपड़े के ऊपर इस्तेमाल किया जाना चाहिए।
4) निर्जलीकरण को रोकने के लिए पीने के लिए बच्चे को बहुत सारे तरल पदार्थ दें। अगर बच्चा है
तेज बुखार और / या तेजी से सांस ले रहा है, यह निर्जलीकरण में जोड़ देगा ।।
5) कमरे में कोई मजबूत गंध नहीं होना चाहिए।
Ans. When children get sick, they look helpless and vulnerable. They may not
complain, but become withdrawn and quiet. A child who should be playing will curl
up in a comer, or become indifferent to everything around. The reason may be fever,
pain or immense tiredness.
The child in your care in the center may fall sick or the parent may bring a sick child
to you for help. You will have for observe the child carefully to see if she is ill and to
determine the extent of illness.
The following are symptoms of mild or moderate illness:
When the child becomes inactive and does not play.
When the child is tired all the time.
When the child cries continuously, or is irritable.
When the child refuses feeds, or is vomiting.
When there is fever with cold and cough.
When there is pain anywhere.
When there is a skin rash with or without fever.
When there is any swelling anywhere.
The following are symptoms of severe illness:
Irritable or listless child, crying or whimpering,
Difficulty in breathing.
Fever with rapid breathing. (More than 50 times per minute)
Drowsy and cannot be roused.
Has fits (convulsions) with or without fever.
Dry lips and sunken eyes. Skin dry and wrinkled.
Not responding to stimuli.
looks bluish, yellowish or very pale
Of course, each illness will have its specific symptoms about which you will read in
the I subsequent Units. But the symptoms described above are general ones, which
indicate tha-9 e child has some health problem.
शिकायत करें, लेकिन वापस लें और शांत हो जाएं। एक बच्चा जो खेल रहा है, वह कर्ल करेगा
एक हास्य में, या चारों ओर सब कुछ के प्रति उदासीन हो जाते हैं। कारण बुखार हो सकता है,
दर्द या अपार थकान।
केंद्र में आपकी देखभाल करने वाला बच्चा बीमार पड़ सकता है या माता-पिता बीमार बच्चे को ला सकते हैं
आपकी मदद के लिए। आपको बच्चे को ध्यान से देखना होगा कि वह बीमार है या नहीं
ब20मारी की सीमा निर्धारित करें।
निम्नलिखित हल्के या मध्यम बीमारी के लक्षण हैं:
जब बच्चा निष्क्रिय हो जाता है और नहीं खेलता है।
जब बच्चा हर समय थका रहता है।
जब बच्चा लगातार रोता है, या चिड़चिड़ा होता है।
जब बच्चा फ़ीड से इनकार करता है, या उल्टी करता है।
जब सर्दी और खांसी के साथ बुखार होता है।
जब कहीं भी दर्द होता है।
जब बुखार के साथ या बिना त्वचा लाल चकत्ते हो।
जब कहीं भी कोई सूजन हो।
निम्नलिखित गंभीर बीमारी के लक्षण हैं:
चिड़चिड़ा या सुनने वाला बच्चा, रोता या फुसफुसाता हुआ,
सांस लेने में कठिनाई।
तेज सांस के साथ बुखार। (प्रति मिनट 50 से अधिक बार)
उखड़ा और उखड़ा नहीं जा सकता।
बुखार के साथ या उसके बिना फिट (ऐंठन) है।
सूखे होंठ और धँसी हुई आँखें। त्वचा सूखी और झुर्रियों वाली।
उत्तेजनाओं का जवाब नहीं।
नीला, पीला या बहुत पीला दिखता है
बेशक, प्रत्येक बीमारी के अपने विशिष्ट लक्षण होंगे जिनके बारे में आप पढ़ेंगे
मैं बाद की इकाइयाँ। लेकिन ऊपर वर्णित लक्षण सामान्य हैं, जो
संकेत था -9 ई बच्चे को कुछ स्वास्थ्य समस्या है।
Q20. What are the general rules in caring for the sick child
reduce the child’s distress and make her rest.
The general rules for treating any chiLd who sick are:
(1) Never leave the child alone in a room. Tell the mother o
older sibling to stay
with the child and talk to her. If the child is not too sick, an older sibling or friend
can play with her.
(2) See that the room is well ventilated. There should not be any draught, but at the
same time there should be fresh air.
() The child’s clothes and bed clothes should be light and clean, preferably of
cotton. Warm clothes, if necessary, should be used over the cotton clothes.
(4) Give plenty of liquids to the child to drink to prevent dehydration. If the child
has high fever and/or is breathing rapidly, this will add to dehydration..
(5) There should be no strong smells in the room.
(6) Treat the symptoms of the illness.
If there is high fever, bring the temperature down with sponging. Put a wet cloth
over the forehead, and when the cloth gets hot, wet it in cold water again. Repeat
until the temperature comes down. If the temperature is very high, tepid’ (room
temperature) sponging of the whole body will help. Gently rub the whole body with
a wet towel, taking care to see that there is no draught in the room.
If there is diarrhoea, start on oral rehydration.
If there is shivering or fits, keep the child well covered.
If there is difficulty in breathing raise the
In fever keep the feet covered and warm.
If there is vomiting, see that the child does not choke on the liquid she brings up.
Turn the head to one side.
If there is vomiting, give a spoonful of sugar
If there is a wound, clean and dress it.
(7)If the child is hungry, give light easily digestible food. Avoid fried and oily food.
(8) Keep the child clean. Clean the mouth with a swab of cotton dipped in glycerin or
even plain water.
(9) Give medication only if you are sure about what has to be given. If needed
contact. The doctor, the Primary Health Centre, the Lady Health Visitor or the
Auxiliary Nurse, Midwife.
(10) Watch for worsening symptoms.
(11) Ensure proper disposal of waste (stools, vomitus) so that the infection does not
spread.
(12) If an infant falls ill and the mother has been breast feeding the child, encourage
her to continue doing so. Many mothers believe that breast feeding the child during
illness is harmful. But this is a wrong notion
उत्तर:। बच्चे की बीमारी जो भी हो, आपको पहले चिड को आराम से करना चाहिए। की कोशिश
बच्चे के संकट को कम करें और उसे आराम दें।
किसी भी चिड के इलाज के सामान्य नियम जो बीमार हैं:
(1) बच्चे को कभी भी एक कमरे में अकेला न छोड़ें। माँ ओ को बताओ
रहने के लिए पुराने भाई-बहन
बच्चे के साथ और उससे बात करें। यदि बच्चा बहुत बीमार नहीं है, तो एक बड़ा भाई या दोस्त
उसके साथ खेल सकते हैं।
(२) देखें कि कमरा अच्छी तरह हवादार है। कोई मसौदा नहीं होना चाहिए, लेकिन
उसी समय ताजी हवा होनी चाहिए।
() बच्चे के कपड़े और बिस्तर के कपड़े हल्के और साफ होने चाहिए, अधिमानतः
कपास। गर्म कपड़े, यदि आवश्यक हो, सूती कपड़े के ऊपर इस्तेमाल किया जाना चाहिए।
(4) निर्जलीकरण को रोकने के लिए बच्चे को बहुत सारे तरल पदार्थ पीने के लिए दें। अगर बच्चा है
तेज बुखार है और / या तेजी से सांस ले रहा है, यह निर्जलीकरण में जोड़ देगा ।।
(५) कमरे में तेज गंध नहीं होना चाहिए।
(6) बीमारी के लक्षणों का इलाज करें।
तेज बुखार होने पर स्पंजिंग के साथ तापमान नीचे लाएं। एक गीला कपड़ा रखो
माथे के ऊपर, और जब कपड़ा गर्म हो जाता है, तो इसे फिर से ठंडे पानी में गीला करें। दोहराना
जब तक तापमान नीचे नहीं आता। यदि तापमान बहुत अधिक है, तो टीपिड ‘(कमरा)
तापमान) पूरे शरीर की स्पंजिंग से मदद मिलेगी। धीरे से पूरे शरीर को रगड़ें
एक गीला तौलिया, यह देखते हुए कि कमरे में कोई मसौदा नहीं है।
दस्त होने पर, मौखिक पुनर्जलीकरण शुरू करें।
अगर कंपकंपी होती है या फिट बैठता है, तो बच्चे को अच्छी तरह से ढक कर रखें।
अगर सांस लेने में कठिनाई हो, तो उठाएं
एक तकिया के साथ सिर।
बुखार में पैरों को ढक कर रखें और गर्म रहें।
यदि उल्टी होती है, तो देखें कि बच्चा उस तरल को चोक नहीं करता है जो वह लाता है।
सिर को एक तरफ मोड़ें।
उल्टी होने पर एक चम्मच चीनी दें
यदि कोई घाव है, तो उसे साफ करें और कपड़े पहनें।
(Child) यदि बच्चा भूखा है, तो उसे आसानी से पचने वाला भोजन दें। तले हुए और तैलीय भोजन से बचें।
(Child) बच्चे को साफ रखें। ग्लिसरीन या में डूबा हुआ कपास की एक झाड़ू के साथ मुंह साफ करें
सादा पानी भी।
(९) दवा तभी दें जब आपको इस बारे में सुनिश्चित हो कि क्या दिया जाना है। अगर जरुरत हो
संपर्क करें। डॉक्टर, प्राथमिक स्वास्थ्य केंद्र, लेडी हेल्थ विजिटर या द
सहायक नर्स, दाई।
(10) बिगड़ते लक्षणों के लिए देखें।
(11) अपशिष्ट (मल, उल्टी) का उचित निपटान सुनिश्चित करें ताकि संक्रमण न हो
फैलाव।
(१२) यदि कोई शिशु बीमार पड़ता है और माँ बच्चे को स्तनपान कराती है, तो उसे प्रोत्साहित करें
उसे ऐसा करना जारी रखना चाहिए। कई माताओं का मानना है कि बच्चे को स्तनपान कराते समय
बीमारी हानिकारक है। लेकिन यह एक गलत धारणा है
Welcome To
Odisha Regional Study Point
We Allows the best competitive exam preparation for SSC,BANKING, RAILWAY &Other State Exam(CT, BE.d) DECE(IGNOU) In ଓଡ଼ିଆ Language…
Why opt ORSP?
✅Daily Free Live class
✅Daily Free practice Quiz
✅FREE Live Tests Quiz
✅Performance Analysis
✅All Govt Exams are Covered
Join With us As per Schedule
And
Happy Learning…
Thank You
ORSP
(9502052059)
Subcribe Youtube Channel Link-
Join Our Telegram Channel(ORSP)
Join Our Telegram Channel(DECE)(IGNOU)
Join Our Telegram Channel(ORSP DISCUSS)
Join Our Telegram Channel(DECE DISCUSS)
Join Our Telegram Channel(JULY 2020)
Thank You
ORSP
9502052059